Page 108 - HIVMED_v21_i1.indb
P. 108
Page 17 of 34 Guideline
Key points
• People who use drugs should be informed of their rights information and commodities tailored to their substance
to confidentiality and consent and their right to refuse use (considering their patterns and type of substance,
HIV testing if they choose. etc.) and sexual practices.
• Uptake and retention in care are improved where ART is • People who use drugs and who test HIV-negative should
integrated with OST when needed. test regularly (every 6 weeks to 3 months) depending on
• Pregnant women living with HIV who are not on ART their risk profile.
should be enrolled on an ART programme urgently.
• Needle-and-syringe programmes and other evidence- • An individual with a discrepant HIV test result should be
based harm reduction services should be offered to all referred for re-testing in 14 days.
people who use drugs, irrespective of their HIV status. • If a person comes for HTS within 72 h after a potential
52
• All people who use drugs and who are found to be HIV- exposure, then PEP should be considered (see section
negative should be provided with risk reduction ‘Pre- and post-exposure prophylaxis’)
2.6 Prevention and management of coinfections and comorbidities
2.6.1 Tuberculosis services
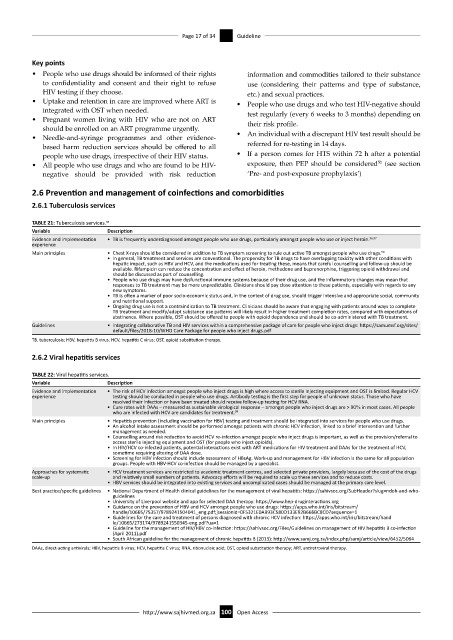
TABLE 21: Tuberculosis services. 98
Variable Description
Evidence and implementation • TB is frequently underdiagnosed amongst people who use drugs, particularly amongst people who use or inject heroin. 96,97
experience
Main principles • Chest X-rays should be considered in addition to TB symptom screening to rule out active TB amongst people who use drugs.
98
• In general, TB treatment and services are conventional. The propensity for TB drugs to have overlapping toxicity with other conditions with
hepatic impact, such as HBV and HCV, and the medications used for treating these, means that careful counselling and follow-up should be
available. Rifampicin can reduce the concentration and effect of heroin, methadone and buprenorphine, triggering opioid withdrawal and
should be discussed as part of counselling.
• People who use drugs may have dysfunctional immune systems because of their drug use, and the inflammatory changes may mean that
responses to TB treatment may be more unpredictable. Clinicians should pay close attention to these patients, especially with regards to any
new symptoms.
• TB is often a marker of poor socio-economic status and, in the context of drug use, should trigger intensive and appropriate social, community
and nutritional support.
• Ongoing drug use is not a contraindication to TB treatment. Clinicians should be aware that engaging with patients around ways to complete
TB treatment and modify/adapt substance use patterns will likely result in higher treatment completion rates, compared with expectations of
abstinence. Where possible, OST should be offered to people with opioid dependence and should be co-administered with TB treatment.
Guidelines • Integrating collaborative TB and HIV services within a comprehensive package of care for people who inject drugs: https://samumsf.org/sites/
default/files/2018-10/WHO Care Package for people who inject drugs.pdf
TB, tuberculosis; HBV, hepatitis B virus; HCV, hepatitis C virus; OST, opioid substitution therapy.
2.6.2 Viral hepatitis services
TABLE 22: Viral hepatitis services.
Variable Description
Evidence and implementation • The risk of HCV infection amongst people who inject drugs is high where access to sterile injecting equipment and OST is limited. Regular HCV
experience testing should be conducted in people who use drugs. Antibody testing is the first step for people of unknown status. Those who have
resolved their infection or have been treated should receive follow-up testing for HCV RNA.
• Cure rates with DAAs – measured as sustainable virological response – amongst people who inject drugs are > 90% in most cases. All people
who are infected with HCV are candidates for treatment.
99
Main principles • Hepatitis prevention (including vaccination for HBV) testing and treatment should be integrated into services for people who use drugs.
• An alcohol intake assessment should be performed amongst patients with chronic HCV infection, linked to a brief intervention and further
management as needed.
• Counselling around risk reduction to avoid HCV re-infection amongst people who inject drugs is important, as well as the provision/referral to
access sterile injecting equipment and OST (for people who inject opioids).
• In HIV/HCV co-infected patients, potential interactions exist with ART medications for HIV treatment and DAAs for the treatment of HCV,
sometime requiring altering of DAA dose.
• Screening for HBV infection should include assessment of HBsAg. Work-up and management for HBV infection is the same for all population
groups. People with HBV-HCV co-infection should be managed by a specialist.
Approaches for systematic • HCV treatment services are restricted to academic treatment centres, and selected private providers, largely because of the cost of the drugs
scale-up and relatively small numbers of patients. Advocacy efforts will be required to scale up these services and to reduce costs.
• HBV services should be integrated into existing services and uncomplicated cases should be managed at the primary care level.
Best practice/specific guidelines • National Department of Health clinical guidelines for the management of viral hepatitis: https://sahivsoc.org/SubHeader?slug=ndoh-and-who-
guidelines
• University of Liverpool website and app for selected DAA therapy: https://www.hep-druginteractions.org
• Guidance on the prevention of HBV and HCV amongst people who use drugs: https://apps.who.int/iris/bitstream/
handle/10665/75357/9789241504041_eng.pdf;jsessionid=0F5321E0AB93C580D133E92B666BC8CD?sequence=1
• Guidelines for the care and treatment of persons diagnosed with chronic HCV infection: https://apps.who.int/iris/bitstream/hand
le/10665/273174/9789241550345-eng.pdf?ua=1
• Guideline for the management of HIV/HBV co-infection: https://sahivsoc.org/Files/Guidelines on management of HIV hepatitis B co-infection
(April 2011).pdf
• South African guideline for the management of chronic hepatitis B (2013): http://www.samj.org.za/index.php/samj/article/view/6452/5064
DAAs, direct-acting antivirals; HBV, hepatitis B virus; HCV, hepatitis C virus; RNA, ribonucleic acid; OST, opioid substitution therapy; ART, antiretroviral therapy.
http://www.sajhivmed.org.za 100 Open Access