Page 104 - HIVMED_v21_i1.indb
P. 104
Page 13 of 34 Guideline
BOX 19: Opioid substitution therapy for special populations. 74,81
Treatment is more complex in children and adolescents, pregnant or breastfeeding women, patients with significant medical comorbidity (e.g. hepatic impairment, HIV, TB and
complex psychiatric pathology) and in patients with chronic pain who are dependent on prescription opioids. It is recommended that such patients be managed together with a
specialist in the treatment of opioid use disorders.
81
TB, tuberculosis.
BOX 20: Management of acute pain in opioid use disorders.
Patients with acute pain and opioid use disorders can be challenging to manage, partly because of central sensitisation, tolerance and opioid-induced hyperalgesia. Clinician-
82
related barriers (including limited knowledge about opioid equivalent doses, stigmatisation and fear of overdose) may lead to poor analgesia in opioid-tolerant patients.
Note: 82
• Pain is not controlled with methadone or buprenorphine for OST as it is dosed daily and the analgesic effect only lasts 4–8 h
• There is no evidence that exposure to opioid analgesics in the presence of acute pain increases rates of reuse of illicit opioids
• The additive effects of opioid analgesics and OST have not been shown to cause clinically significant respiratory or central nervous system depression
• Reports of acute pain with objective findings are unlikely to be manipulative gestures
• Additional guidance is provided in Appendix 3.
Source: Developed by Dr Urvisha Bhoora, a participant of the guideline workshop, for this guideline, drawing from the cited references
OST, opioid substitution therapy.
2.4.3 Overdose services
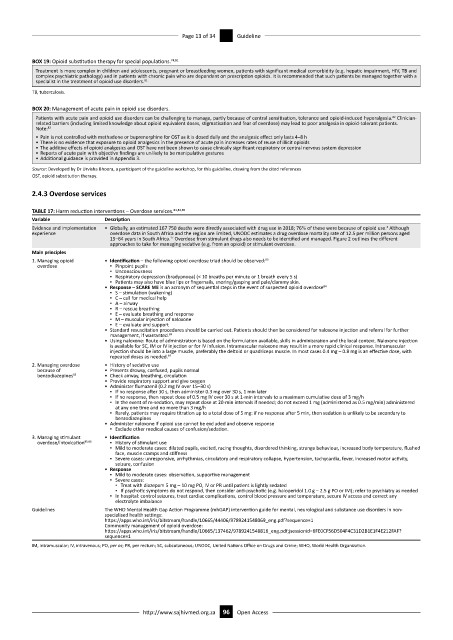
TABLE 17: Harm reduction interventions – Overdose services. 83,84,85
Variable Description
2
Evidence and implementation • Globally, an estimated 167 750 deaths were directly associated with drug use in 2018; 76% of these were because of opioid use. Although
experience overdose data in South Africa and the region are limited, UNODC estimates a drug overdose mortality rate of 12.5 per million persons aged
17
15–64 years in South Africa. Overdose from stimulant drugs also needs to be identified and managed. Figure 2 outlines the different
approaches to take for managing sedative (e.g. from an opioid) or stimulant overdose.
Main principles
1. Managing opioid • Identification – the following opioid overdose triad should be observed: 83
overdose ▪ Pinpoint pupils
▪ Unconsciousness
▪ Respiratory depression (bradypnoea) (< 10 breaths per minute or 1 breath every 5 s)
▪ Patients may also have blue lips or fingernails, snoring/gasping and pale/clammy skin.
• Response – SCARE ME is an acronym of sequential steps in the event of suspected opioid overdose 84
▪ S – stimulation (wakening)
▪ C – call for medical help
▪ A – airway
▪ R – rescue breathing
▪ E – evaluate breathing and response
▪ M – muscular injection of naloxone
▪ E – evaluate and support
• Standard resuscitation procedures should be carried out. Patients should then be considered for naloxone injection and referral for further
management, if warranted. 84
• Using naloxone: Route of administration is based on the formulation available, skills in administration and the local context. Naloxone injection
is available for SC, IM or IV injection or for IV infusion. Intramuscular naloxone may result in a more rapid clinical response. Intramuscular
injection should be into a large muscle, preferably the deltoid or quadriceps muscle. In most cases 0.4 mg – 0.8 mg is an effective dose, with
repeated doses as needed. 84
2. Managing overdose • History of sedative use
because of • Presents drowsy, confused, pupils normal
benzodiazepines 85 • Check airway, breathing, circulation
• Provide respiratory support and give oxygen
• Administer flumazenil (0.2 mg IV over 15–30 s)
▪ If no response after 30 s, then administer 0.3 mg over 30 s, 1 min later
▪ If no response, then repeat dose of 0.5 mg IV over 30 s at 1-min intervals to a maximum cumulative dose of 3 mg/h
▪ In the event of re-sedation, may repeat dose at 20-min intervals if needed; do not exceed 1 mg (administered as 0.5 mg/min) administered
at any one time and no more than 3 mg/h
▪ Rarely, patients may require titration up to a total dose of 5 mg: if no response after 5 min, then sedation is unlikely to be secondary to
benzodiazepines
• Administer naloxone if opioid use cannot be excluded and observe response
▪ Exclude other medical causes of confusion/sedation.
3. Managing stimulant • Identification
overdose/intoxication 85,86 ▪ History of stimulant use
▪ Mild to moderate cases: dilated pupils, excited, racing thoughts, disordered thinking, strange behaviour, increased body temperature, flushed
face, muscle cramps and stiffness
▪ Severe cases: unresponsive, arrhythmias, circulatory and respiratory collapse, hypertension, tachycardia, fever, increased motor activity,
seizure, confusion
• Response
▪ Mild to moderate cases: observation, supportive management
▪ Severe cases:
▪ Treat with diazepam 5 mg – 10 mg PO, IV or PR until patient is lightly sedated
▪ If psychotic symptoms do not respond, then consider anti-psychotic (e.g. haloperidol 1.0 g – 2.5 g PO or IM); refer to psychiatry as needed
▪ In hospital: control seizures, treat cardiac complications, control blood pressure and temperature, secure IV access and correct any
electrolyte imbalance
Guidelines The WHO Mental Health Gap Action Programme (mhGAP) intervention guide for mental, neurological and substance use disorders in non-
specialised health settings:
https://apps.who.int/iris/bitstream/handle/10665/44406/9789241548069_eng.pdf?sequence=1
Community management of opioid overdose:
https://apps.who.int/iris/bitstream/handle/10665/137462/9789241548816_eng.pdf;jsessionid=6FE0CF56D504F4C31D2B1E1F4E212FAF?
sequence=1
IM, intramuscular; IV, intravenous; PO, per os; PR, per rectum; SC, subcutaneous; UNODC, United Nations Office on Drugs and Crime; WHO, World Health Organization.
http://www.sajhivmed.org.za 96 Open Access