Page 101 - HIVMED_v21_i1.indb
P. 101
Page 10 of 34 Guideline
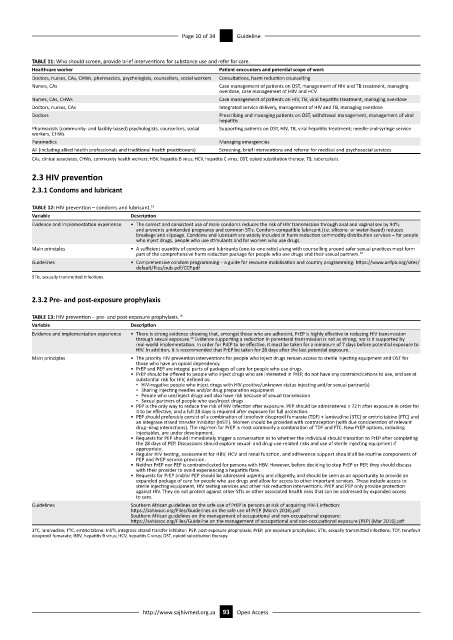
TABLE 11: Who should screen, provide brief interventions for substance use and refer for care.
Healthcare worker Patient encounters and potential scope of work
Doctors, nurses, CAs, CHWs, pharmacists, psychologists, counsellors, social workers Consultations, harm reduction counselling
Nurses, CAs Case management of patients on OST, management of HIV and TB treatment, managing
overdose, case management of HBV and HCV
Nurses, CAs, CHWs Case management of patients on HIV, TB, viral hepatitis treatment, managing overdose
Doctors, nurses, CAs Integrated service delivery, management of HIV and TB, managing overdose
Doctors Prescribing and managing patients on OST, withdrawal management, management of viral
hepatitis
Pharmacists (community- and facility-based) psychologists, counsellors, social Supporting patients on OST, HIV, TB, viral hepatitis treatment; needle-and-syringe service
workers, CHWs
Paramedics Managing emergencies
All (including allied health professionals and traditional health practitioners) Screening, brief interventions and referral for medical and psychosocial services
CAs, clinical associates; CHWs, community health workers; HBV, hepatitis B virus; HCV, hepatitis C virus; OST, opioid substitution therapy; TB, tuberculosis.
2.3 HIV prevention
2.3.1 Condoms and lubricant
TABLE 12: HIV prevention – condoms and lubricant. 19
Variable Description
Evidence and implementation experience • The correct and consistent use of male condoms reduces the risk of HIV transmission through anal and vaginal sex by 94%
and prevents unintended pregnancy and common STIs. Condom-compatible lubricant (i.e. silicone- or water-based) reduces
breakage and slippage. Condoms and lubricant are widely included in harm reduction commodity distribution services – for people
who inject drugs, people who use stimulants and for women who use drugs.
Main principles • A sufficient quantity of condoms and lubricants (one-to-one ratio) along with counselling around safer sexual practices must form
part of the comprehensive harm reduction package for people who use drugs and their sexual partners. 19
Guidelines • Comprehensive condom programming – a guide for resource mobilisation and country programming: https://www.unfpa.org/sites/
default/files/pub-pdf/CCP.pdf
STIs, sexually transmitted infections.
2.3.2 Pre- and post-exposure prophylaxis
TABLE 13: HIV prevention – pre- and post-exposure prophylaxis. 19
Variable Description
Evidence and implementation experience • There is strong evidence showing that, amongst those who are adherent, PrEP is highly effective in reducing HIV transmission
19
through sexual exposure. Evidence supporting a reduction in parenteral transmission is not as strong, nor is it supported by
real-world implementation. In order for PrEP to be effective, it must be taken for a minimum of 7 days before potential exposure to
HIV. In addition, it is recommended that PrEP be taken for 28 days after the last potential exposure.
Main principles • The priority HIV prevention interventions for people who inject drugs remain access to sterile injecting equipment and OST for
those who have an opioid dependency.
• PrEP and PEP are integral parts of packages of care for people who use drugs.
• PrEP should be offered to people who inject drugs who are interested in PrEP, do not have any contraindications to use, and are at
substantial risk for HIV, defined as:
▪ HIV-negative people who inject drugs with HIV-positive/unknown status injecting and/or sexual partner(s)
▪ Sharing injecting needles and/or drug preparation equipment
▪ People who use/inject drugs and also have risk because of sexual transmission
▪ Sexual partners of people who use/inject drugs
• PEP is the only way to reduce the risk of HIV infection after exposure. PEP should be administered ≤ 72 h after exposure in order for
it to be effective, and a full 28 days is required after exposure for full protection.
• PEP should preferably consist of a combination of tenofovir disoproxil fumarate (TDF) + lamivudine (3TC) or emtricitabine (FTC) and
an integrase strand transfer inhibitor (InSTI). Women should be provided with contraception (with due consideration of relevant
drug–drug interactions). The regimen for PrEP is most commonly a combination of TDF and FTC. New PrEP options, including
injectables, are under development.
• Requests for PEP should immediately trigger a conversation as to whether the individual should transition to PrEP after completing
the 28 days of PEP. Discussions should explore sexual- and drug-use-related risks and use of sterile injecting equipment if
appropriate.
• Regular HIV testing, assessment for HBV, HCV and renal function, and adherence support should all be routine components of
PEP and PrEP service provision.
• Neither PrEP nor PEP is contraindicated for persons with HBV. However, before deciding to stop PrEP or PEP, they should discuss
with their provider to avoid experiencing a hepatitis flare.
• Requests for PrEP and/or PEP should be addressed urgently and diligently, and should be seen as an opportunity to provide an
expanded package of care for people who use drugs and allow for access to other important services. These include access to
sterile injecting equipment, HIV testing services and other risk reduction interventions. PrEP and PEP only provide protection
against HIV. They do not protect against other STIs or other associated health risks that can be addressed by expanded access
to care.
Guidelines Southern African guidelines on the safe use of PrEP in persons at risk of acquiring HIV-1 infection:
https://sahivsoc.org/Files/Guidelines on the safe use of PrEP (March 2016).pdf
Southern African guidelines on the management of occupational and non-occupational exposure:
https://sahivsoc.org/Files/Guideline on the management of occupational and non-occupational exposure (PEP) (Mar 2016).pdf
3TC, lamivudine; FTC, emtricitabine; InSTI, integrase strand transfer inhibitor; PEP, post-exposure prophylaxis; PrEP, pre-exposure prophylaxis; STIs, sexually transmitted infections; TDF, tenofovir
disoproxil fumarate; HBV, hepatitis B virus; HCV, hepatitis C virus; OST, opioid substitution therapy.
http://www.sajhivmed.org.za 93 Open Access