Page 99 - HIVMED_v21_i1.indb
P. 99
Page 8 of 34 Guideline
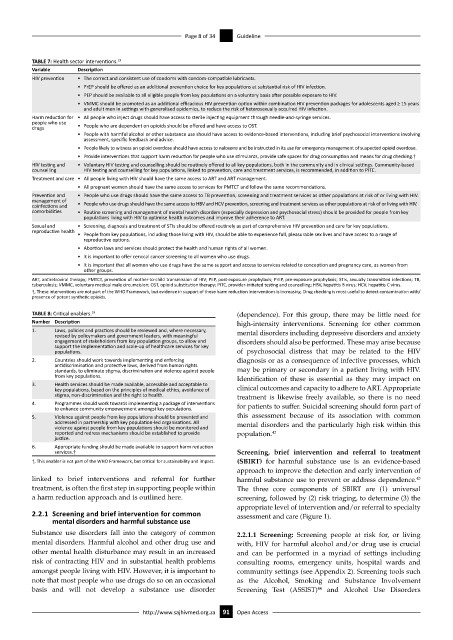
TABLE 7: Health sector interventions. 19
Variable Description
HIV prevention • The correct and consistent use of condoms with condom-compatible lubricants.
• PrEP should be offered as an additional prevention choice for key populations at substantial risk of HIV infection.
• PEP should be available to all eligible people from key populations on a voluntary basis after possible exposure to HIV.
• VMMC should be promoted as an additional efficacious HIV prevention option within combination HIV prevention packages for adolescents aged ≥ 15 years
and adult men in settings with generalised epidemics, to reduce the risk of heterosexually acquired HIV infection.
Harm reduction for • All people who inject drugs should have access to sterile injecting equipment through needle-and-syringe services.
people who use
drugs • People who are dependent on opioids should be offered and have access to OST.
• People with harmful alcohol or other substance use should have access to evidence-based interventions, including brief psychosocial interventions involving
assessment, specific feedback and advice.
• People likely to witness an opioid overdose should have access to naloxone and be instructed in its use for emergency management of suspected opioid overdose.
• Provide interventions that support harm reduction for people who use stimulants, provide safe spaces for drug consumption and means for drug checking.†
HIV testing and • Voluntary HIV testing and counselling should be routinely offered to all key populations, both in the community and in clinical settings. Community-based
counselling HIV testing and counselling for key populations, linked to prevention, care and treatment services, is recommended, in addition to PITC.
Treatment and care • All people living with HIV should have the same access to ART and ART management.
• All pregnant women should have the same access to services for PMTCT and follow the same recommendations.
Prevention and • People who use drugs should have the same access to TB prevention, screening and treatment services as other populations at risk of or living with HIV.
management of
coinfections and • People who use drugs should have the same access to HBV and HCV prevention, screening and treatment services as other populations at risk of or living with HIV.
comorbidities • Routine screening and management of mental health disorders (especially depression and psychosocial stress) should be provided for people from key
populations living with HIV to optimise health outcomes and improve their adherence to ART.
Sexual and • Screening, diagnosis and treatment of STIs should be offered routinely as part of comprehensive HIV prevention and care for key populations.
reproductive health
• People from key populations, including those living with HIV, should be able to experience full, pleasurable sex lives and have access to a range of
reproductive options.
• Abortion laws and services should protect the health and human rights of all women.
• It is important to offer cervical cancer screening to all women who use drugs.
• It is important that all women who use drugs have the same support and access to services related to conception and pregnancy care, as women from
other groups.
ART, antiretroviral therapy; PMTCT, prevention of mother-to-child transmission of HIV; PEP, post-exposure prophylaxis; PrEP, pre-exposure prophylaxis; STIs, sexually transmitted infections; TB,
tuberculosis; VMMC, voluntary medical male circumcision; OST, opioid substitution therapy; PITC, provider-initiated testing and counselling; HBV, hepatitis B virus; HCV, hepatitis C virus.
†, These interventions are not part of the WHO Framework, but evidence in support of these harm reduction interventions is increasing. Drug checking is most useful to detect contamination with/
presence of potent synthetic opioids.
TABLE 8: Critical enablers. 19 (dependence). For this group, there may be little need for
Number Description high-intensity interventions. Screening for other common
1. Laws, policies and practices should be reviewed and, where necessary, mental disorders including depressive disorders and anxiety
revised by policymakers and government leaders, with meaningful
engagement of stakeholders from key population groups, to allow and disorders should also be performed. These may arise because
support the implementation and scale-up of healthcare services for key
populations. of psychosocial distress that may be related to the HIV
2. Countries should work towards implementing and enforcing diagnosis or as a consequence of infective processes, which
antidiscrimination and protective laws, derived from human rights
standards, to eliminate stigma, discrimination and violence against people may be primary or secondary in a patient living with HIV.
from key populations. Identification of these is essential as they may impact on
3. Health services should be made available, accessible and acceptable to
key populations, based on the principles of medical ethics, avoidance of clinical outcomes and capacity to adhere to ART. Appropriate
stigma, non-discrimination and the right to health. treatment is likewise freely available, so there is no need
4. Programmes should work towards implementing a package of interventions for patients to suffer. Suicidal screening should form part of
to enhance community empowerment amongst key populations.
5. Violence against people from key populations should be prevented and this assessment because of its association with common
addressed in partnership with key population-led organisations. All mental disorders and the particularly high risk within this
violence against people from key populations should be monitored and
reported and redress mechanisms should be established to provide population. 42
justice.
6. Appropriate funding should be made available to support harm reduction
services.† Screening, brief intervention and referral to treatment
†, This enabler is not part of the WHO Framework, but critical for sustainability and impact. (SBIRT) for harmful substance use is an evidence-based
approach to improve the detection and early intervention of
linked to brief interventions and referral for further harmful substance use to prevent or address dependence.
43
treatment, is often the first step in supporting people within The three core components of SBIRT are (1) universal
a harm reduction approach and is outlined here. screening, followed by (2) risk triaging, to determine (3) the
appropriate level of intervention and/or referral to specialty
2.2.1 Screening and brief intervention for common assessment and care (Figure 1).
mental disorders and harmful substance use
Substance use disorders fall into the category of common 2.2.1.1 Screening: Screening people at risk for, or living
mental disorders. Harmful alcohol and other drug use and with, HIV for harmful alcohol and/or drug use is crucial
other mental health disturbance may result in an increased and can be performed in a myriad of settings including
risk of contracting HIV and in substantial health problems consulting rooms, emergency units, hospital wards and
amongst people living with HIV. However, it is important to community settings (see Appendix 2). Screening tools such
note that most people who use drugs do so on an occasional as the Alcohol, Smoking and Substance Involvement
basis and will not develop a substance use disorder Screening Test (ASSIST) and Alcohol Use Disorders
44
http://www.sajhivmed.org.za 91 Open Access