Page 103 - HIVMED_v21_i1.indb
P. 103
Page 12 of 34 Guideline
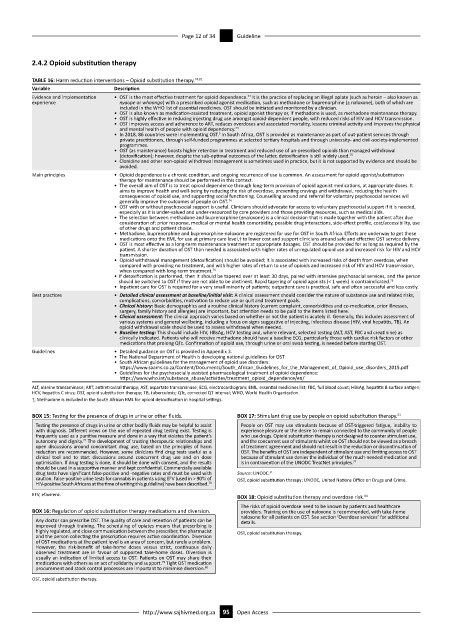
2.4.2 Opioid substitution therapy
TABLE 16: Harm reduction interventions – Opioid substitution therapy. 74,81
Variable Description
Evidence and implementation • OST is the most effective treatment for opioid dependence. It is the practice of replacing an illegal opiate (such as heroin – also known as
74
experience nyaope or whoonga) with a prescribed opioid agonist medication, such as methadone or buprenorphine (± naloxone), both of which are
included in the WHO list of essential medicines. OST should be initiated and monitored by a clinician.
• OST is also known as medication-assisted treatment, opioid agonist therapy or, if methadone is used, as methadone maintenance therapy.
• OST is highly effective in reducing injecting drug use amongst opioid-dependent people, with reduced risks of HIV and HCV transmission.
• OST improves access and adherence to ART, reduces overdoses and associated mortality, lessens criminal activity and improves the physical
and mental health of people with opioid dependency. 74
• In 2018, 86 countries were implementing OST. In South Africa, OST is provided as maintenance as part of out-patient services through
5
private practitioners, through self-funded programmes at selected tertiary hospitals and through university- and civil-society-implemented
programmes.
• OST (as maintenance) boasts higher retention in treatment and reduced use of un-prescribed opioids than managed withdrawal
(detoxification); however, despite the sub-optimal outcomes of the latter, detoxification is still widely used. 75
• Clonidine and other non-opioid withdrawal management is sometimes used in practice, but it is not supported by evidence and should be
avoided.
Main principles • Opioid dependence is a chronic condition, and ongoing recurrence of use is common. An assessment for opioid agonist/substitution
therapy for maintenance should be performed in this context.
• The overall aim of OST is to treat opioid dependence through long-term provision of opioid agonist medications, at appropriate doses. It
aims to improve health and well-being by reducing the risk of overdose, preventing cravings and withdrawal, reducing the health
consequences of opioid use, and supporting social functioning. Counselling around and referral for voluntary psychosocial services will
generally improve the outcomes of people on OST.
74
• OST with or without psychosocial support is useful. Clinicians should advocate for access to voluntary psychosocial support if it is needed,
especially as it is under-valued and under-resourced by care providers and those providing resources, such as medical aids.
• The selection between methadone and buprenorphine (±naloxone) is a clinical decision that is made together with the patient after due
consideration of: prior response, medical or mental health comorbidity, possible drug interactions, side-effect profile, cost/accessibility, use
of other drugs and patient choice.
• Methadone, buprenorphine and buprenorphine-naloxone are registered for use for OST in South Africa. Efforts are underway to get these
medications onto the EML for use at primary care level,† to lower cost and support clinicians around safe and effective OST service delivery.
• OST is most effective as a long-term maintenance treatment at appropriate dosages. OST should be provided for as long as required by the
patient. A shorter duration of OST than needed is associated with higher rates of unregulated opioid use and increased risk for HIV and HCV
transmission.
• Opioid withdrawal management (detoxification) should be avoided; it is associated with increased risks of death from overdose, when
compared with providing no treatment, and with higher rates of return to use of opioids and increased risk of HIV and HCV transmission,
when compared with long-term treatment.
76
• If detoxification is performed, then it should be tapered over at least 30 days, paired with intensive psychosocial services, and the person
should be switched to OST if they are not able to be abstinent. Rapid tapering of opioid agonists (< 1 week) is contraindicated. 75
• Inpatient care for OST is required for a very small minority of patients; outpatient care is practical, safe and often successful and less costly.
Best practices • Detailed clinical assessment at baseline/initial visit: A clinical assessment should consider the nature of substance use and related risks,
complications, comorbidities, motivation to reduce use or quit and treatment goals.
• Clinical history: Basic demographics and a routine clinical history (current complaint, comorbidities and co-medication, prior illnesses,
surgery, family history and allergies) are important, but attention needs to be paid to the items listed here.
• Clinical assessment: The clinical approach varies based on whether or not the patient is acutely ill. Generally, this includes assessment of
various systems and general wellbeing, including a focus on signs suggestive of injecting, infectious disease (HIV, viral hepatitis, TB). An
opioid withdrawal scale should be used to assess withdrawal when needed.
• Baseline testing: This should include HIV, HBsAg, HCV testing and, where relevant, selected testing (ALT, AST, FBC and creatinine) as
clinically indicated. Patients who will receive methadone should have a baseline ECG, particularly those with cardiac risk factors or other
medications that prolong QTc. Confirmation of opioid use, through urine or oral swab testing, is needed before starting OST.
Guidelines • Detailed guidance on OST is provided in Appendix 3.
• The National Department of Health is developing national guidelines for OST
• South African guidelines for the management of opioid use disorders:
https://www.saams.co.za/Content/Documents/South_African_Guidelines_for_the_Management_of_Opioid_use_disorders_2015.pdf
• Guidelines for the psychosocially assisted pharmacological treatment of opioid dependence:
https://www.who.int/substance_abuse/activities/treatment_opioid_dependence/en/
ALT, alanine transaminase; ART, antiretroviral therapy; AST, aspartate transaminase; ECG, electrocardiogram; EML, essential medicines list; FBC, full blood count; HBsAg, hepatitis B surface antigen;
HCV, hepatitis C virus; OST, opioid substitution therapy; TB, tuberculosis; QTc, corrected QT interval; WHO, World Health Organization.
†, Methadone is included in the South African EML for opioid detoxification in hospital settings.
BOX 15: Testing for the presence of drugs in urine or other fluids. BOX 17: Stimulant drug use by people on opioid substitution therapy. 51
Testing the presence of drugs in urine or other bodily fluids may be helpful to assist People on OST may use stimulants because of OST-triggered fatigue, inability to
with diagnosis. Different views on the use of repeated drug testing exist. Testing is experience pleasure or the desire to remain connected to the community of people
frequently used as a punitive measure and done in a way that violates the patient’s who use drugs. Opioid substitution therapy is not designed to counter stimulant use,
autonomy and dignity. The development of trusting therapeutic relationships and and the concurrent use of stimulants whilst on OST should not be viewed as a breach
77
open discussions around concomitant drug use, based on the principles of harm of treatment agreement and should not result in the reduction or discontinuation of
reduction are recommended. However, some clinicians find drug tests useful as a OST. The benefits of OST are independent of stimulant use and limiting access to OST
clinical tool and to start discussions around concurrent drug use and on dose because of stimulant use denies the individual of the much-needed medication and
optimisation. If drug testing is done, it should be done with consent, and the results is in contravention of the UNODC TreatNet principles. 77
should be used in a supportive manner and kept confidential. Commercially available
drug tests have significant false-positive and -negative rates and must be used with Source: UNODC. 51
caution. False-positive urine tests for cannabis in patients using EFV (used in > 90% of OST, opioid substitution therapy; UNODC, United Nations Office on Drugs and Crime.
HIV-positive South Africans at the time of writing this guideline) have been described.
78
EFV, efavirenz. 84
BOX 18: Opioid substitution therapy and overdose risk.
The risks of opioid overdose need to be known by patients and healthcare
BOX 16: Regulation of opioid substitution therapy medications and diversion. providers. Training on the use of naloxone is recommended, with take-home
naloxone for all patients on OST. See section ‘Overdose services’ for additional
Any doctor can prescribe OST. The quality of care and retention of patients can be details.
improved through training. The scheduling of opiates means that prescribing is
highly regulated, and close communication between the prescriber, the pharmacist OST, opioid substitution therapy.
and the person collecting the prescription requires active coordination. Diversion
of OST medications at the patient level is an area of concern, but rarely a problem.
However, the risk-benefit of take-home doses versus strict, continuous daily
observed treatment are in favour of supported take-home doses. Diversion is
usually an indication of limited access to OST. Patients on OST may share their
79
medications with others as an act of solidarity and support. Tight OST medication
procurement and stock control processes are important to minimise diversion. 80
OST, opioid substitution therapy.
http://www.sajhivmed.org.za 95 Open Access