Page 107 - HIVMED_v21_i1.indb
P. 107
Page 16 of 34 Guideline
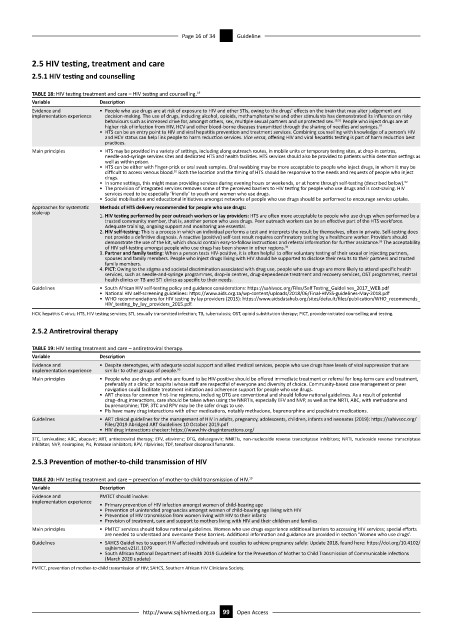
2.5 HIV testing, treatment and care
2.5.1 HIV testing and counselling
TABLE 18: HIV testing treatment and care – HIV testing and counselling. 19
Variable Description
Evidence and • People who use drugs are at risk of exposure to HIV and other STIs, owing to the drugs’ effects on the brain that may alter judgement and
implementation experience decision-making. The use of drugs, including alcohol, opioids, methamphetamine and other stimulants has demonstrated its influence on risky
behaviours such as increased drive for, amongst others, sex, multiple sexual partners and unprotected sex. 19,51 People who inject drugs are at
higher risk of infection from HIV, HCV and other blood-borne diseases transmitted through the sharing of needles and syringes.
19
• HTS can be an entry point to HIV and viral hepatitis prevention and treatment services. Combining counselling with knowledge of a person’s HIV
and HCV status can help link people to harm reduction services. Vice versa, offering HIV and viral hepatitis testing is part of harm reduction best
practices.
Main principles • HTS may be provided in a variety of settings, including along outreach routes, in mobile units or temporary testing sites, at drop-in centres,
needle-and-syringe services sites and dedicated HTS and health facilities. HTS services should also be provided to patients within detention settings as
well as within prison.
• HTS can be either with finger-prick or oral swab samples. Oral swabbing may be more acceptable to people who inject drugs, in whom it may be
52
difficult to access venous blood. Both the location and the timing of HTS should be responsive to the needs and requests of people who inject
drugs.
52
• In some settings, this might mean providing services during evening hours or weekends, or at home through self-testing (described below).
• The provision of integrated services removes some of the perceived barriers to HIV testing for people who use drugs and is cost-saving. HIV
services need to be especially ‘friendly’ to youth and women who use drugs.
• Social mobilisation and educational initiatives amongst networks of people who use drugs should be performed to encourage service uptake.
Approaches for systematic Methods of HTS delivery recommended for people who use drugs:
scale-up
1. HIV testing performed by peer outreach workers or lay providers: HTS are often more acceptable to people who use drugs when performed by a
trusted community member, that is, another person who uses drugs. Peer outreach workers can be an effective part of the HTS workforce.
Adequate training, ongoing support and monitoring are essential.
2. HIV self-testing: This is a process in which an individual performs a test and interprets the result by themselves, often in private. Self-testing does
not provide a definitive diagnosis. A reactive (positive) self-test result requires confirmatory testing by a healthcare worker. Providers should
demonstrate the use of the kit, which should contain easy-to-follow instructions and referral information for further assistance. The acceptability
93
of HIV self-testing amongst people who use drugs has been shown in other regions.
94
3. Partner and family testing: When a person tests HIV-positive, it is often helpful to offer voluntary testing of their sexual or injecting partners,
spouses and family members. People who inject drugs living with HIV should be supported to disclose their results to their partners and trusted
family members.
4. PICT: Owing to the stigma and societal discrimination associated with drug use, people who use drugs are more likely to attend specific health
services, such as needle-and-syringe programmes, drop-in centres, drug-dependence treatment and recovery services, OST programmes, mental
health clinics or TB and STI clinics as specific to their needs.
Guidelines • South African HIV self-testing policy and guidance considerations: https://sahivsoc.org/Files/Self Testing_Guidelines_2017_WEB.pdf
• National HIV self-screening guidelines: https://www.aids.org.za/wp-content/uploads/2018/06/Final-HIVSS-guidelines-May-2018.pdf
• WHO recommendations for HIV testing by lay providers (2015): https://www.aidsdatahub.org/sites/default/files/publication/WHO_recommends_
HIV_testing_by_lay_providers_2015.pdf.
HCV, hepatitis C virus; HTS, HIV testing services; STI, sexually transmitted infection; TB, tuberculosis; OST, opioid substitution therapy; PICT, provider-initiated counselling and testing.
2.5.2 Antiretroviral therapy
TABLE 19: HIV testing treatment and care – antiretroviral therapy.
Variable Description
Evidence and • Despite stereotypes, with adequate social support and allied medical services, people who use drugs have levels of viral suppression that are
implementation experience similar to other groups of people. 95
Main principles • People who use drugs and who are found to be HIV-positive should be offered immediate treatment or referral for long-term care and treatment,
preferably at a clinic or hospital whose staff are respectful of everyone and diversity of choice. Community-based case management or peer
navigation could facilitate treatment initiation and adherence support for people who use drugs.
• ART choices for common first-line regimens, including DTG are conventional and should follow national guidelines. As a result of potential
drug–drug interactions, care should be taken when using the NNRTIs, especially EFV and NVP, as well as the NRTI, ABC, with methadone and
buprenorphine; TDF, 3TC and RPV may be the safer drugs to use.
• PIs have many drug interactions with other medications, notably methadone, buprenorphine and psychiatric medications.
Guidelines • ART clinical guidelines for the management of HIV in adults, pregnancy, adolescents, children, infants and neonates (2019): https://sahivsoc.org/
Files/2019 Abridged ART Guidelines 10 October 2019.pdf
• HIV drug interactions checker: https://www.hiv-druginteractions.org/
3TC, lamivudine; ABC, abacavir; ART, antiretroviral therapy; EFV, efavirenz; DTG, dolutegravir; NNRTIs, non-nucleoside reverse transcriptase inhibitors; NRTI, nucleoside reverse transcriptase
inhibitor; NVP, nevirapine; PIs, Protease inhibitors; RPV, rilpivirine; TDF, tenofovir disoproxil fumarate.
2.5.3 Prevention of mother-to-child transmission of HIV
TABLE 20: HIV testing treatment and care – prevention of mother-to-child transmission of HIV. 19
Variable Description
Evidence and PMTCT should involve:
implementation experience
• Primary prevention of HIV infection amongst women of child-bearing age
• Prevention of unintended pregnancies amongst women of child-bearing age living with HIV
• Prevention of HIV transmission from women living with HIV to their infants
• Provision of treatment, care and support to mothers living with HIV and their children and families
Main principles • PMTCT services should follow national guidelines. Women who use drugs experience additional barriers to accessing HIV services; special efforts
are needed to understand and overcome these barriers. Additional information and guidance are provided in section ‘Women who use drugs’.
Guidelines • SAHCS Guidelines to support HIV-affected individuals and couples to achieve pregnancy safely: Update 2018, found here: https://doi.org/10.4102/
sajhivmed.v21i1.1079
• South African National Department of Health 2019 Guideline for the Prevention of Mother to Child Transmission of Communicable Infections
(March 2020 update)
PMTCT, prevention of mother-to-child transmission of HIV; SAHCS, Southern African HIV Clinicians Society.
http://www.sajhivmed.org.za 99 Open Access