Page 111 - HIVMED_v21_i1.indb
P. 111
Page 20 of 34 Guideline
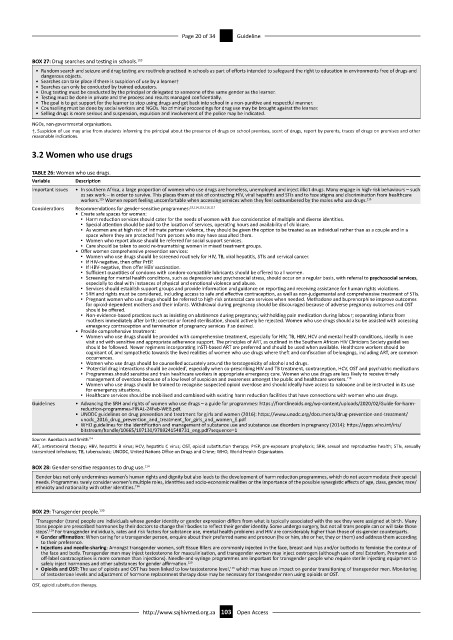
BOX 27: Drug searches and testing in schools. 113
• Random search and seizure and drug testing are routinely practised in schools as part of efforts intended to safeguard the right to education in environments free of drugs and
dangerous objects.
• Searches can take place if there is suspicion of use by a learner†
• Searches can only be conducted by trained educators.
• Drug testing must be conducted by the principal or delegated to someone of the same gender as the learner.
• Testing must be done in private and the process and results managed confidentially.
• The goal is to get support for the learner to stop using drugs and get back into school in a non-punitive and respectful manner.
• Counselling must be done by social workers and NGOs. No criminal proceedings for drug use may be brought against the learner.
• Selling drugs is more serious and suspension, expulsion and involvement of the police may be indicated.
NGOs, non-governmental organisations.
†, Suspicion of use may arise from students informing the principal about the presence of drugs on school premises, scent of drugs, report by parents, traces of drugs on premises and other
reasonable indications.
3.2 Women who use drugs
TABLE 26: Women who use drugs.
Variable Description
Important issues • In southern Africa, a large proportion of women who use drugs are homeless, unemployed and inject illicit drugs. Many engage in high-risk behaviours – such
as sex work – in order to survive. This places them at risk of contracting HIV, viral hepatitis and STIs and to face stigma and discrimination from healthcare
workers. Women report feeling uncomfortable when accessing services when they feel outnumbered by the males who use drugs. 115
115
Considerations Recommendations for gender-sensitive programmes: 19,114,115,116,117
• Create safe spaces for women:
▪ Harm reduction services should cater for the needs of women with due consideration of multiple and diverse identities.
▪ Special attention should be paid to the location of services, operating hours and availability of childcare.
▪ As women are at high risk of intimate partner violence, they should be given the option to be treated as an individual rather than as a couple and in a
space where they are protected from persons who may have assaulted them.
▪ Women who report abuse should be referred for social support services.
▪ Care should be taken to avoid re-traumatising women in mixed treatment groups.
• Offer women comprehensive prevention services:
▪ Women who use drugs should be screened routinely for HIV, TB, viral hepatitis, STIs and cervical cancer.
▪ If HIV-negative, then offer PrEP.
▪ If HBV-negative, then offer HBV vaccination.
▪ Sufficient quantities of condoms with condom-compatible lubricants should be offered to all women.
▪ Screening for mental health conditions, such as depression and psychosocial stress, should occur on a regular basis, with referral to psychosocial services,
especially to deal with instances of physical and emotional violence and abuse.
▪ Services should establish support groups and provide information and guidance on reporting and receiving assistance for human rights violations.
▪ SRH and rights must be considered, including access to safe and effective contraception, as well as non-judgemental and comprehensive treatment of STIs.
▪ Pregnant women who use drugs should be referred to high-risk antenatal care services when needed. Methadone and buprenorphine improve outcomes
for opioid-dependent mothers and their infants. Withdrawal during pregnancy should be discouraged because of adverse pregnancy outcomes and OST
should be offered.
▪ Non-evidence-based practices such as insisting on abstinence during pregnancy; withholding pain medication during labour; separating infants from
mothers immediately after birth; coerced or forced sterilisation, should actively be rejected. Women who use drugs should also be assisted with accessing
emergency contraception and termination of pregnancy services if so desired.
• Provide comprehensive treatment:
▪ Women who use drugs should be provided with comprehensive treatment, especially for HIV, TB, HBV, HCV and mental health conditions, ideally in one
visit and with sensitive and appropriate adherence support. The principles of ART, as outlined in the Southern African HIV Clinicians Society guidelines
should be followed. Newer regimens incorporating InSTI-based ART are preferred and should be used when available. Healthcare workers should be
cognisant of, and sympathetic towards the lived realities of women who use drugs where theft and confiscation of belongings, including ART, are common
occurrences.
▪ Women who use drugs should be counselled accurately around the teratogenicity of alcohol and drugs.
▪ ‘Potential drug interactions should be avoided’, especially when co-prescribing HIV and TB treatment, contraception, HCV, OST and psychiatric medications
▪ Programmes should sensitise and train healthcare workers in appropriate emergency care. Women who use drugs are less likely to receive timely
management of overdose because of a low level of suspicion and awareness amongst the public and healthcare workers.
118
▪ Women who use drugs should be trained to recognise suspected opioid overdose and should ideally have access to naloxone and be instructed in its use
for emergency situations.
▪ Healthcare services should be mobilised and combined with existing harm reduction facilities that have connections with women who use drugs.
Guidelines • Advancing the SRH and rights of women who use drugs – a guide for programmes: https://frontlineaids.org/wp-content/uploads/2020/02/Guide-for-harm-
reduction-programmes-FINAL-24Feb-WEB.pdf.
• UNODC guidelines on drug prevention and treatment for girls and women (2016): https://www.unodc.org/documents/drug-prevention-and-treatment/
unodc_2016_drug_prevention_and_treatment_for_girls_and_women_E.pdf
• WHO guidelines for the identification and management of substance use and substance use disorders in pregnancy (2014): https://apps.who.int/iris/
bitstream/handle/10665/107130/9789241548731_eng.pdf?sequence=1
Source: Auerbach and Smith 114
ART, antiretroviral therapy; HBV, hepatitis B virus; HCV, hepatitis C virus; OST, opioid substitution therapy; PrEP, pre-exposure prophylaxis; SRH, sexual and reproductive health; STIs, sexually
transmitted infections; TB, tuberculosis; UNODC, United Nations Office on Drugs and Crime; WHO, World Health Organization.
BOX 28: Gender-sensitive responses to drug use. 114
Gender bias not only undermines women’s human rights and dignity but also leads to the development of harm reduction programmes, which do not accommodate their special
needs. Programmes rarely consider women’s multiple roles, identities and socio-economic realities or the importance of the possible synergistic effects of age, class, gender, race/
ethnicity and nationality with other identities.
114
BOX 29: Transgender people. 120
‘Transgender (trans) people are individuals whose gender identity or gender expression differs from what is typically associated with the sex they were assigned at birth. Many
trans people are prescribed hormones by their doctors to change their bodies to reflect their gender identity. Some undergo surgery, but not all trans people can or will take those
steps’. For transgender individuals, rates and risk factors for substance use, mental health problems and HIV are considerably higher than those of cis-gender counterparts.
119
• Gender affirmation: When caring for a transgender person, enquire about their preferred name and pronoun (he or him, she or her, they or them) and address them according
to their preference.
• Injections and needle-sharing: Amongst transgender women, soft tissue fillers are commonly injected in the face, breast and hips and/or buttocks to feminise the contour of
the face and body. Transgender men may inject testosterone for masculinisation, and transgender women may inject oestrogen (although use of oral Estrofem, Premarin and
off-label contraceptives is more common than injections). Needle-and-syringe programmes are important for transgender people who require sterile injecting equipment to
safely inject hormones and other substances for gender affirmation. 120
• Opioids and OST: The use of opioids and OST has been linked to low testosterone level, which may have an impact on gender transitioning of transgender men. Monitoring
120
of testosterone levels and adjustment of hormone replacement therapy dose may be necessary for transgender men using opioids or OST.
OST, opioid substitution therapy.
http://www.sajhivmed.org.za 103 Open Access