Page 112 - HIVMED_v21_i1.indb
P. 112
Page 21 of 34 Guideline
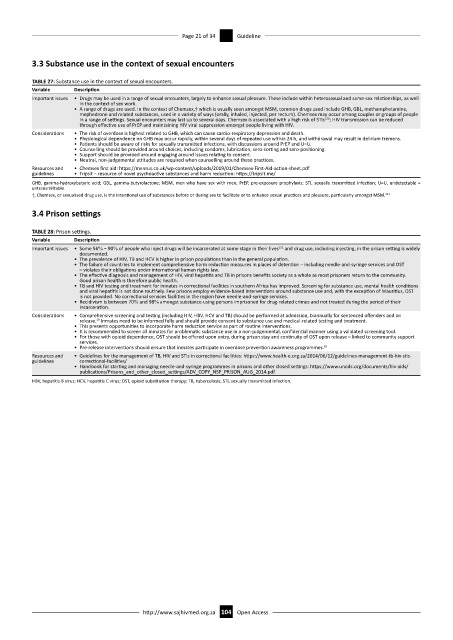
3.3 Substance use in the context of sexual encounters
TABLE 27: Substance use in the context of sexual encounters.
Variable Description
Important issues • Drugs may be used in a range of sexual encounters, largely to enhance sexual pleasure. These include within heterosexual and same-sex relationships, as well
in the context of sex work.
• A range of drugs are used. In the context of Chemsex,† which is usually seen amongst MSM, common drugs used include GHB, GBL, methamphetamine,
mephedrone and related substances, used in a variety of ways (orally, inhaled, injected, per rectum). Chemsex may occur among couples or groups of people
120
in a range of settings. Sexual encounters may last up to several days. Chemsex is associated with a high risk of STIs ; HIV transmission can be reduced
through effective use of PrEP and maintaining HIV viral suppression amongst people living with HIV.
Considerations • The risk of overdose is highest related to GHB, which can cause cardio-respiratory depression and death.
• Physiological dependence on GHB may occur rapidly, within several days of repeated use within 24 h, and withdrawal may result in delirium tremens.
• Patients should be aware of risks for sexually transmitted infections, with discussions around PrEP and U=U.
• Counselling should be provided around choices, including condoms, lubrication, sero-sorting and sero-positioning.
• Support should be provided around engaging around issues relating to consent.
• Neutral, non-judgemental attitudes are required when counselling around these practices.
Resources and • Chemsex first aid: https://menrus.co.uk/wp-content/uploads/2019/01/Chemsex-First-Aid-action-sheet.pdf
guidelines • Tripsit – resource of novel psychoactive substances and harm reduction: https://tripsit.me/
GHB, gamma-hydroxybutyric acid; GBL, gamma-butyrolactone; MSM, men who have sex with men; PrEP, pre-exposure prophylaxis; STI, sexually transmitted infection; U=U, undetectable =
untransmittable.
121
†, Chemsex, or sexualised drug use, is the intentional use of substances before or during sex to facilitate or to enhance sexual practices and pleasure, particularly amongst MSM.
3.4 Prison settings
TABLE 28: Prison settings.
Variable Description
122
Important issues • Some 56% – 90% of people who inject drugs will be incarcerated at some stage in their lives and drug use, including injecting, in the prison setting is widely
documented.
• The prevalence of HIV, TB and HCV is higher in prison populations than in the general population.
• The failure of countries to implement comprehensive harm reduction measures in places of detention – including needle-and-syringe services and OST
– violates their obligations under international human rights law.
• The effective diagnosis and management of HIV, viral hepatitis and TB in prisons benefits society as a whole as most prisoners return to the community.
Good prison health is therefore public health.
• TB and HIV testing and treatment for inmates in correctional facilities in southern Africa has improved. Screening for substance use, mental health conditions
and viral hepatitis is not done routinely. Few prisons employ evidence-based interventions around substance use and, with the exception of Mauritius, OST
is not provided. No correctional services facilities in the region have needle-and-syringe services.
• Recidivism is between 70% and 98% amongst substance-using persons imprisoned for drug-related crimes and not treated during the period of their
incarceration.
Considerations • Comprehensive screening and testing (including HIV, HBV, HCV and TB) should be performed at admission, biannually for sentenced offenders and on
release. Inmates need to be informed fully and should provide consent to substance use and medical-related testing and treatment.
19
• This presents opportunities to incorporate harm reduction service as part of routine interventions.
• It is recommended to screen all inmates for problematic substance use in a non-judgemental, confidential manner using a validated screening tool.
• For those with opioid dependence, OST should be offered upon entry, during prison stay and continuity of OST upon release – linked to community support
services.
• Pre-release interventions should ensure that inmates participate in overdose prevention awareness programmes. 83
Resources and • Guidelines for the management of TB, HIV and STIs in correctional facilities: https://www.health-e.org.za/2014/06/12/guidelines-management-tb-hiv-stis-
guidelines correctional-facilities/
• Handbook for starting and managing needle-and-syringe programmes in prisons and other closed settings: https://www.unodc.org/documents/hiv-aids/
publications/Prisons_and_other_closed_settings/ADV_COPY_NSP_PRISON_AUG_2014.pdf
HBV, hepatitis B virus; HCV, hepatitis C virus; OST, opioid substitution therapy; TB, tuberculosis; STI, sexually transmitted infection.
http://www.sajhivmed.org.za 104 Open Access