Page 109 - HIVMED_v21_i1.indb
P. 109
Page 18 of 34 Guideline
2.6.3 Mental health services 2.7 Critical enablers
2.7.1 Supportive law and policy
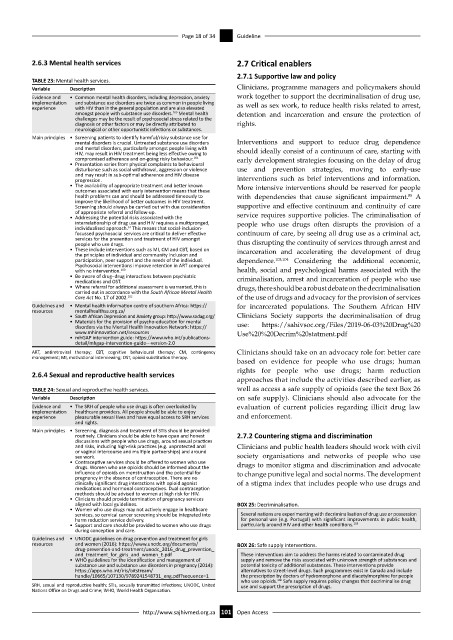
TABLE 23: Mental health services.
Variable Description Clinicians, programme managers and policymakers should
Evidence and • Common mental health disorders, including depression, anxiety work together to support the decriminalisation of drug use,
implementation and substance use disorders are twice as common in people living as well as sex work, to reduce health risks related to arrest,
experience with HIV than in the general population and are also elevated
100
amongst people with substance use disorders. Mental health detention and incarceration and ensure the protection of
challenges may be the result of psychosocial stress related to the
diagnosis or other factors or may be directly attributed to rights.
neurological or other opportunistic infections or substances.
Main principles • Screening patients to identify harmful/risky substance use for
mental disorders is crucial. Untreated substance use disorders Interventions and support to reduce drug dependence
and mental disorders, particularly amongst people living with should ideally consist of a continuum of care, starting with
HIV, may result in HIV treatment being less effective owing to
compromised adherence and on-going risky behaviour. 101 early development strategies focusing on the delay of drug
• Presentation varies from physical complaints to behavioural
disturbance such as social withdrawal, aggression or violence use and prevention strategies, moving to early-use
and may result in sub-optimal adherence and HIV disease
progression. interventions such as brief interventions and information.
• The availability of appropriate treatment and better known More intensive interventions should be reserved for people
outcomes associated with early intervention means that these
health problems can and should be addressed timeously to with dependencies that cause significant impairment. A
85
improve the likelihood of better outcomes in HIV treatment.
Screening should always be carried out with due consideration supportive and effective continuum and continuity of care
of appropriate referral and follow-up. service requires supportive policies. The criminalisation of
• Addressing the potential risks associated with the
interrelationship of drug use and HIV requires a multipronged, people who use drugs often disrupts the provision of a
individualised approach. This means that social-inclusion-
57
focussed psychosocial services are critical to deliver effective continuum of care, by seeing all drug use as a criminal act,
services for the prevention and treatment of HIV amongst
people who use drugs. thus disrupting the continuity of services through arrest and
• These include interventions such as MI, CM and CBT, based on incarceration and accelerating the development of drug
the principles of individual and community inclusion and
participation, peer support and the needs of the individual. dependence. 103,104 Considering the additional economic,
Psychosocial interventions improve retention in ART compared
with no intervention. 100 health, social and psychological harms associated with the
• Be aware of drug–drug interactions between psychiatric criminalisation, arrest and incarceration of people who use
medications and OST.
• Where referral for additional assessment is warranted, this is drugs, there should be a robust debate on the decriminalisation
carried out in accordance with the South African Mental Health
Care Act No. 17 of 2002. 102 of the use of drugs and advocacy for the provision of services
Guidelines and • Mental health information centre of southern Africa: https:// for incarcerated populations. The Southern African HIV
resources mentalhealthsa.org.za/
• South African Depression and Anxiety group: http://www.sadag.org/ Clinicians Society supports the decriminalisation of drug
• Materials for the provision of psycho-education for mental use: https://sahivsoc.org/Files/2019-06-03%20Drug%20
disorders via the Mental Health Innovation Network: https://
www.mhinnovation.net/resources Use%20%20Decrim%20statment.pdf
• mhGAP intervention guide: https://www.who.int/publications-
detail/mhgap-intervention-guide---version-2.0
ART, antiretroviral therapy; CBT, cognitive behavioural therapy; CM, contingency Clinicians should take on an advocacy role for: better care
management; MI, motivational interviewing; OST, opioid substitution therapy.
based on evidence for people who use drugs; human
rights for people who use drugs; harm reduction
2.6.4 Sexual and reproductive health services
approaches that include the activities described earlier, as
TABLE 24: Sexual and reproductive health services. well as access a safe supply of opioids (see the text Box 26
Variable Description on safe supply). Clinicians should also advocate for the
Evidence and • The SRH of people who use drugs is often overlooked by evaluation of current policies regarding illicit drug law
implementation healthcare providers. All people should be able to enjoy
experience pleasurable sexual lives and have equal access to SRH services and enforcement.
and rights.
Main principles • Screening, diagnosis and treatment of STIs should be provided
routinely. Clinicians should be able to have open and honest 2.7.2 Countering stigma and discrimination
discussions with people who use drugs, around sexual practices
and risks, including high-risk practices (e.g. unprotected anal Clinicians and public health leaders should work with civil
or vaginal intercourse and multiple partnerships) and around
sex work. society organisations and networks of people who use
• Contraceptive services should be offered to women who use drugs to monitor stigma and discrimination and advocate
drugs. Women who use opioids should be informed about the
influence of opioids on menstruation and the potential for to change punitive legal and social norms. The development
pregnancy in the absence of contraception. There are no
clinically significant drug interactions with opioid agonist of a stigma index that includes people who use drugs and
medications and hormonal contraceptives. Dual contraception
methods should be advised to women at high risk for HIV.
• Clinicians should provide termination of pregnancy services
aligned with local guidelines. BOX 25: Decriminalisation.
• Women who use drugs may not actively engage in healthcare
services, so cervical cancer screening should be integrated into Several nations are experimenting with decriminalisation of drug use or possession
harm reduction service delivery. for personal use (e.g. Portugal) with significant improvements in public health,
105
• Support and care should be provided to women who use drugs particularly around HIV and other health conditions.
during conception and care.
Guidelines and • UNODC guidelines on drug prevention and treatment for girls
resources and women (2016): https://www.unodc.org/documents/ BOX 26: Safe supply interventions.
drug-prevention-and-treatment/unodc_2016_drug_prevention_
and_treatment_for_girls_and_women_E.pdf These interventions aim to address the harms related to contaminated drug
• WHO guidelines for the identification and management of supply and remove the risks associated with unknown strength of substances and
substance use and substance use disorders in pregnancy (2014): potential toxicity of additional substances. These interventions provide
https://apps.who.int/iris/bitstream/ alternatives to street-level drugs. Such programmes exist in Canada and include
handle/10665/107130/9789241548731_eng.pdf?sequence=1 the prescription by doctors of hydromorphone and diacetylmorphine for people
who use opioids. Safe supply requires policy changes that decriminalise drug
106
SRH, sexual and reproductive health; STIs, sexually transmitted infections; UNODC, United use and support the prescription of drugs.
Nations Office on Drugs and Crime; WHO, World Health Organization.
http://www.sajhivmed.org.za 101 Open Access