Page 113 - HIVMED_v21_i1.indb
P. 113
Page 22 of 34 Guideline
4. Recommendations
This section summarises the key role of critical stakeholders in the delivery of harm reduction services in HIV, TB, viral hepatitis
and related services.
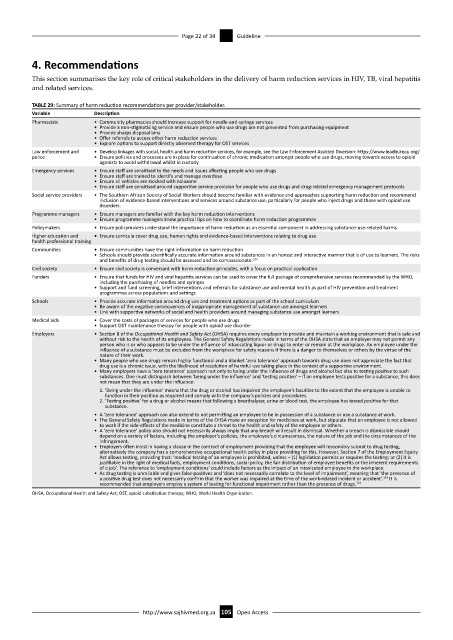
TABLE 29: Summary of harm reduction recommendations per provider/stakeholder.
Variable Description
Pharmacists • Community pharmacies should increase support for needle-and-syringe services
• Provide a non-stigmatising service and ensure people who use drugs are not prevented from purchasing equipment
• Provide sharps disposal bins
• Offer referrals to access other harm reduction services
• Explore options to support directly observed therapy for OST services
Law enforcement and • Develop linkages with social, health and harm reduction services, for example, see the Law Enforcement Assisted Diversion: https://www.leadbureau.org/
police • Ensure policies and processes are in place for continuation of chronic medication amongst people who use drugs, moving towards access to opioid
agonists to avoid withdrawal whilst in custody
Emergency services • Ensure staff are sensitised to the needs and issues affecting people who use drugs
• Ensure staff are trained to identify and manage overdose
• Ensure all vehicles are stocked with naloxone
• Ensure staff are sensitised around supportive service provision for people who use drugs and drug-related emergency management protocols
Social service providers • The Southern African Society of Social Workers should become familiar with evidence and approaches supporting harm reduction and recommend
inclusion of evidence-based interventions and services around substance use, particularly for people who inject drugs and those with opioid use
disorders.
Programme managers • Ensure managers are familiar with the key harm reduction interventions
• Ensure programme managers know practical tips on how to coordinate harm reduction programmes
Policymakers • Ensure policymakers understand the importance of harm reduction as an essential component in addressing substance-use-related harms.
Higher education and • Ensure curricula cover drug use, human rights and evidence-based interventions relating to drug use
health professional training
Communities • Ensure communities have the right information on harm reduction
• Schools should provide scientifically accurate information around substances in an honest and interactive manner that is of use to learners. The risks
and benefits of drug testing should be assessed and be compassionate. 123
Civil society • Ensure civil society is conversant with harm reduction principles, with a focus on practical application
Funders • Ensure that funds for HIV and viral hepatitis services can be used to cover the full package of comprehensive services recommended by the WHO,
including the purchasing of needles and syringes
• Support and fund screening, brief interventions and referrals for substance use and mental health as part of HIV prevention and treatment
programmes across populations and settings
Schools • Provide accurate information around drug use and treatment options as part of the school curriculum
• Be aware of the negative consequences of inappropriate management of substance use amongst learners
• Link with supportive networks of social and health providers around managing substance use amongst learners
Medical aids • Cover the costs of packages of services for people who use drugs
• Support OST maintenance therapy for people with opioid use disorder
Employers • Section 8 of the Occupational Health and Safety Act (OHSA) requires every employer to provide and maintain a working environment that is safe and
without risk to the health of its employees. The General Safety Regulations made in terms of the OHSA state that an employer may not permit any
person who is or who appears to be under the influence of intoxicating liquor or drugs to enter or remain at the workplace. An employee under the
influence of a substance must be excluded from the workplace for safety reasons if there is a danger to themselves or others by the virtue of the
nature of their work.
• Many people who use drugs remain highly functional and a blanket ‘zero tolerance’ approach towards drug use does not appreciate the fact that
drug use is a chronic issue, with the likelihood of resolution of harmful use taking place in the context of a supportive environment.
• Many employers have a ‘zero tolerance’ approach not only to being under the influence of drugs and alcohol but also to testing positive to such
substances. One must distinguish between ‘being under the influence’ and ‘testing positive’ – if an employee tests positive for a substance, this does
not mean that they are under the influence:
1. ‘Being under the influence’ means that the drug or alcohol has impaired the employee’s faculties to the extent that the employee is unable to
function in their position as required and comply with the company’s policies and procedures.
2. ‘Testing positive’ for a drug or alcohol means that following a breathalyser, urine or blood test, the employee has tested positive for that
substance.
• A ‘zero tolerance’ approach can also extend to not permitting an employee to be in possession of a substance or use a substance at work.
• The General Safety Regulations made in terms of the OHSA make an exception for medicines at work, but stipulate that an employee is not allowed
to work if the side-effects of the medicine constitute a threat to the health and safety of the employee or others.
• A ‘zero tolerance’ policy also should not necessarily always imply that any breach will result in dismissal. Whether a breach is dismissible should
depend on a variety of factors, including the employer’s policies, the employee’s circumstances, the nature of the job and the circumstances of the
infringement.
• Employers often insist in having a clause in the contract of employment providing that the employee will reasonably submit to drug testing,
alternatively the company has a comprehensive occupational health policy in place providing for this. However, Section 7 of the Employment Equity
Act allows testing, providing that: ‘medical testing of an employee is prohibited, unless – (1) legislation permits or requires the testing; or (2) it is
justifiable in the light of medical facts, employment conditions, social policy, the fair distribution of employee benefits or the inherent requirements
of a job’. The reference to ‘employment conditions’ could include factors as the impact of an intoxicated employee in the workplace.
• As drug testing is unreliable and gives false-positives and ‘does not necessarily correlate to the level of impairment’, meaning that ‘the presence of
124
a positive drug test does not necessarily confirm that the worker was impaired at the time of the work-related incident or accident’. It is
recommended that employers employ a system of testing for functional impairment rather than the presence of drugs. 124
OHSA, Occupational Health and Safety Act; OST, opioid substitution therapy; WHO, World Health Organization.
http://www.sajhivmed.org.za 105 Open Access