Page 102 - HIVMED_v21_i1.indb
P. 102
Page 11 of 34 Guideline
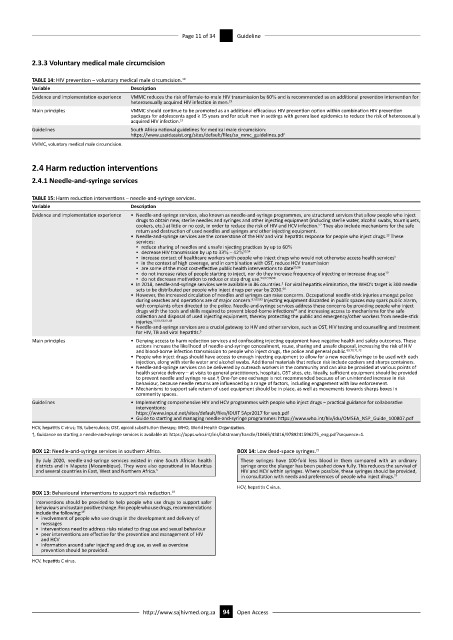
2.3.3 Voluntary medical male circumcision
TABLE 14: HIV prevention – voluntary medical male circumcision. 19
Variable Description
Evidence and implementation experience VMMC reduces the risk of female-to-male HIV transmission by 60% and is recommended as an additional prevention intervention for
heterosexually acquired HIV infection in men. 19
Main principles VMMC should continue to be promoted as an additional efficacious HIV prevention option within combination HIV prevention
packages for adolescents aged ≥ 15 years and for adult men in settings with generalised epidemics to reduce the risk of heterosexually
19
acquired HIV infection.
Guidelines South Africa national guidelines for medical male circumcision:
https://www.usaidassist.org/sites/default/files/sa_mmc_guidelines.pdf
VMMC, voluntary medical male circumcision.
2.4 Harm reduction interventions
2.4.1 Needle-and-syringe services
TABLE 15: Harm reduction interventions – needle-and-syringe services.
Variable Description
Evidence and implementation experience • Needle-and-syringe services, also known as needle-and-syringe programmes, are structured services that allow people who inject
drugs to obtain new, sterile needles and syringes and other injecting equipment (including sterile water, alcohol swabs, tourniquets,
52
cookers, etc.) at little or no cost, in order to reduce the risk of HIV and HCV infection. They also include mechanisms for the safe
return and destruction of used needles and syringes and other injecting equipment.
23
• Needle-and-syringe services are the cornerstone of the HIV and viral hepatitis response for people who inject drugs. These
services:
▪ reduce sharing of needles and unsafe injecting practices by up to 60%
▪ decrease HIV transmission by up to 33% – 42% 53,54
▪ increase contact of healthcare workers with people who inject drugs who would not otherwise access health services 5
▪ in the context of high coverage, and in combination with OST, reduce HCV transmission
▪ are some of the most cost-effective public health interventions to date 55,56
▪ do not increase rates of people starting to inject, nor do they increase frequency of injecting or increase drug use 19
▪ do not decrease motivation to reduce or stop drug use. 54,57,58,59
• In 2018, needle-and-syringe services were available in 86 countries. For viral hepatitis elimination, the WHO’s target is 300 needle
5
sets to be distributed per people who inject drugs per year by 2030. 60
• However, the increased circulation of needles and syringes can raise concerns. Occupational needle-stick injuries amongst police
during searches and operations are of major concern. 61,62,63 Injecting equipment discarded in public spaces may spark public alarm,
with complaints often directed to the police. Needle-and-syringe services address these concerns by providing people who inject
drugs with the tools and skills required to prevent blood-borne infections and increasing access to mechanisms for the safe
64
collection and disposal of used injecting equipment, thereby protecting the public and emergency/other workers from needle-stick
injuries. 52,65,66,67,68
• Needle-and-syringe services are a crucial gateway to HIV and other services, such as OST, HIV testing and counselling and treatment
for HIV, TB and viral hepatitis. 5
Main principles • Denying access to harm reduction services and confiscating injecting equipment have negative health and safety outcomes. These
actions increase the likelihood of needle-and-syringe concealment, reuse, sharing and unsafe disposal, increasing the risk of HIV
and blood-borne infection transmission to people who inject drugs, the police and general public. 69,70,71,72
• People who inject drugs should have access to enough injecting equipment to allow for a new needle/syringe to be used with each
injection, along with sterile water and alcohol swabs. Additional materials that reduce risk include cookers and sharps containers.
• Needle-and-syringe services can be delivered by outreach workers in the community and can also be provided at various points of
health service delivery – at visits to general practitioners, hospitals, OST sites, etc. Ideally, sufficient equipment should be provided
to prevent needle and syringe re-use.† One-for-one exchange is not recommended because of an unintended increase in risk
behaviour, because needle returns are influenced by a range of factors, including engagement with law enforcement.
• Mechanisms to support safe return of used equipment should be in place, as well as movements towards sharps boxes in
community spaces.
Guidelines • Implementing comprehensive HIV and HCV programmes with people who inject drugs – practical guidance for collaborative
interventions:
https://www.inpud.net/sites/default/files/IDUIT 5Apr2017 for web.pdf
• Guide to starting and managing needle-and-syringe programmes: https://www.who.int/hiv/idu/OMSEA_NSP_Guide_100807.pdf
HCV, hepatitis C virus; TB, tuberculosis; OST, opioid substitution therapy; WHO, World Health Organization.
†, Guidance on starting a needle-and-syringe services is available at: https://apps.who.int/iris/bitstream/handle/10665/43816/9789241596275_eng.pdf?sequence=1.
BOX 12: Needle-and-syringe services in southern Africa. BOX 14: Low dead-space syringes. 73
By July 2020, needle-and-syringe services existed in nine South African health These syringes have 100-fold less blood in them compared with an ordinary
districts and in Maputo (Mozambique). They were also operational in Mauritius syringe once the plunger has been pushed down fully. This reduces the survival of
and several countries in East, West and Northern Africa. 5 HIV and HCV within syringes. Where possible, these syringes should be provided,
in consultation with needs and preferences of people who inject drugs. 73
HCV, hepatitis C virus.
BOX 13: Behavioural interventions to support risk reduction. 19
Interventions should be provided to help people who use drugs to support safer
behaviours and sustain positive change. For people who use drugs, recommendations
include the following: 19
• involvement of people who use drugs in the development and delivery of
messages
• interventions need to address risks related to drug use and sexual behaviour
• peer interventions are effective for the prevention and management of HIV
and HCV
• information around safer injecting and drug use, as well as overdose
prevention should be provided.
HCV, hepatitis C virus.
http://www.sajhivmed.org.za 94 Open Access