Page 49 - HIVMED_v21_i1.indb
P. 49
Page 23 of 39 Guideline
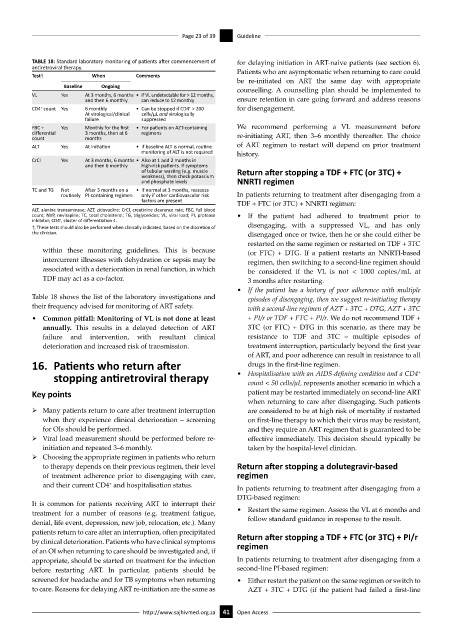
TABLE 18: Standard laboratory monitoring of patients after commencement of for delaying initiation in ART-naive patients (see section 6).
antiretroviral therapy. Patients who are asymptomatic when returning to care could
Test† When Comments
be re-initiated on ART the same day with appropriate
Baseline Ongoing counselling. A counselling plan should be implemented to
VL Yes At 3 months, 6 months • If VL undetectable for > 12 months,
and then 6 monthly can reduce to 12 monthly ensure retention in care going forward and address reasons
CD4 count Yes 6 monthly • Can be stopped if CD4 > 200 for disengagement.
+
+
At virological/clinical cells/µL and virologically
failure suppressed
FBC + Yes Monthly for the first • For patients on AZT-containing We recommend performing a VL measurement before
differential 3 months, then at 6 regimens re-initiating ART, then 3–6 monthly thereafter. The choice
count months
ALT Yes At initiation • If baseline ALT is normal, routine of ART regimen to restart will depend on prior treatment
monitoring of ALT is not required history.
CrCl Yes At 3 months, 6 months • Also at 1 and 2 months in
and then 6 monthly high-risk patients. If symptoms
of tubular wasting (e.g. muscle Return after stopping a TDF + FTC (or 3TC) +
weakness), then check potassium
and phosphate levels NNRTI regimen
TC and TG Not After 3 months on a • If normal at 3 months, reassess
routinely PI-containing regimen only if other cardiovascular risk In patients returning to treatment after disengaging from a
factors are present TDF + FTC (or 3TC) + NNRTI regimen:
ALT, alanine transaminase; AZT, zidovudine; CrCl, creatinine clearance rate; FBC, full blood
count; NVP, nevirapine; TC, total cholesterol; TG, triglycerides; VL, viral load; PI, protease • If the patient had adhered to treatment prior to
inhibitor; CD4 , cluster of differentiation 4.
+
†, These tests should also be performed when clinically indicated, based on the discretion of disengaging, with a suppressed VL, and has only
the clinician. disengaged once or twice, then he or she could either be
restarted on the same regimen or restarted on TDF + 3TC
within these monitoring guidelines. This is because (or FTC) + DTG. If a patient restarts an NNRTI-based
intercurrent illnesses with dehydration or sepsis may be regimen, then switching to a second-line regimen should
associated with a deterioration in renal function, in which be considered if the VL is not < 1000 copies/mL at
TDF may act as a co-factor. 3 months after restarting.
• If the patient has a history of poor adherence with multiple
Table 18 shows the list of the laboratory investigations and episodes of disengaging, then we suggest re-initiating therapy
their frequency advised for monitoring of ART safety. with a second-line regimen of AZT + 3TC + DTG, AZT + 3TC
• Common pitfall: Monitoring of VL is not done at least + PI/r or TDF + FTC + PI/r. We do not recommend TDF +
annually. This results in a delayed detection of ART 3TC (or FTC) + DTG in this scenario, as there may be
failure and intervention, with resultant clinical resistance to TDF and 3TC – multiple episodes of
deterioration and increased risk of transmission. treatment interruption, particularly beyond the first year
of ART, and poor adherence can result in resistance to all
16. Patients who return after drugs in the first-line regimen.
stopping antiretroviral therapy • Hospitalisation with an AIDS-defining condition and a CD4
+
count < 50 cells/μL represents another scenario in which a
Key points patient may be restarted immediately on second-line ART
when returning to care after disengaging. Such patients
ÿ Many patients return to care after treatment interruption are considered to be at high risk of mortality if restarted
when they experience clinical deterioration – screening on first-line therapy to which their virus may be resistant,
for OIs should be performed. and they require an ART regimen that is guaranteed to be
ÿ Viral load measurement should be performed before re- effective immediately. This decision should typically be
initiation and repeated 3–6 monthly. taken by the hospital-level clinician.
ÿ Choosing the appropriate regimen in patients who return
to therapy depends on their previous regimen, their level Return after stopping a dolutegravir-based
of treatment adherence prior to disengaging with care, regimen
and their current CD4 and hospitalisation status. In patients returning to treatment after disengaging from a
+
DTG-based regimen:
It is common for patients receiving ART to interrupt their
treatment for a number of reasons (e.g. treatment fatigue, • Restart the same regimen. Assess the VL at 6 months and
denial, life event, depression, new job, relocation, etc.). Many follow standard guidance in response to the result.
patients return to care after an interruption, often precipitated Return after stopping a TDF + FTC (or 3TC) + PI/r
by clinical deterioration. Patients who have clinical symptoms regimen
of an OI when returning to care should be investigated and, if
appropriate, should be started on treatment for the infection In patients returning to treatment after disengaging from a
before restarting ART. In particular, patients should be second-line PI-based regimen:
screened for headache and for TB symptoms when returning • Either restart the patient on the same regimen or switch to
to care. Reasons for delaying ART re-initiation are the same as AZT + 3TC + DTG (if the patient had failed a first-line
http://www.sajhivmed.org.za 41 Open Access