Page 54 - HIVMED_v21_i1.indb
P. 54
Page 28 of 39 Guideline
20. Liver disease ÿ Using 3TC without TDF to treat HBV/HIV co-infection
Antiretroviral dose adjustment in liver leads to HBV resistance in 80% – 90% of patients after
5 years of treatment.
impairment ÿ Interruption of TDF and/or 3TC (or FTC) has been
Key points associated with flares of life-threatening hepatitis in
patients with hepatitis B in case reports.
ÿ There is no single blood test for accurate quantification of ÿ Adjust dosing frequency of TDF in patients with HBV
liver impairment. infection and renal dysfunction; if renal function is severe
ÿ Child–Pugh class C may require dose adjustment for or deteriorates with TDF, then 3TC monotherapy or other
some ART drugs. drugs with anti-HBV activity should be considered.
ÿ The combination of TDF + 3TC (or FTC) + DTG (or RAL)
is regarded as least hepatotoxic. Hepatitis B virus is a common co-infection with HIV in
southern Africa, with significant implications for progression
Antiretroviral dose adjustments to cirrhosis, as well as for treatment options. Access to
Table 23 shows the outline of dose adjustments for the vaccination, laboratory resources and treatment options is
relevant ART drugs in patients with Child–Pugh class C liver limited to some extent in southern African countries, and the
impairment. recommendations below should be considered in the light of
the local context.
Hepatitis B and human immunodeficiency virus
co-infection Hepatitis B virus and HIV co-infection is associated with:
Key points • an increased risk of chronic liver disease
• a higher HBV VL
ÿ All HIV-infected individuals should be screened for • diminished responses to HBV vaccine
active HBV – hepatitis B surface antigen (HBsAg) • an increased risk of drug-induced hepatotoxicity
screening is an appropriate test. • a flare of hepatitis within 3 months of commencing ART
ÿ The HBV VL correlates with disease progression and is (because of HBV-related IRIS, which is difficult to
used to monitor anti-HBV therapy. differentiate from drug hepatotoxicity).
ÿ All children and adults eligible for HBV vaccination
should be vaccinated. Drugs directed against HBV that have no or minimal anti-HIV
ÿ Antiretroviral therapy drugs with anti-HBV activity are activity (e.g. entecavir and telbivudine) are largely unavailable
TDF + 3TC (or FTC). or extremely expensive in southern African region. Instead, it
ÿ For all HIV-infected HBsAg-positive patients, the ART is usually necessary to use ART drugs that also have anti-HBV
regimen should include TDF + 3TC (or FTC). activity: TDF + 3TC (or FTC). As with HIV, these drugs
suppress HBV but do not eradicate it. Effective treatment
prevents or slows the progression to cirrhosis. For all HIV-
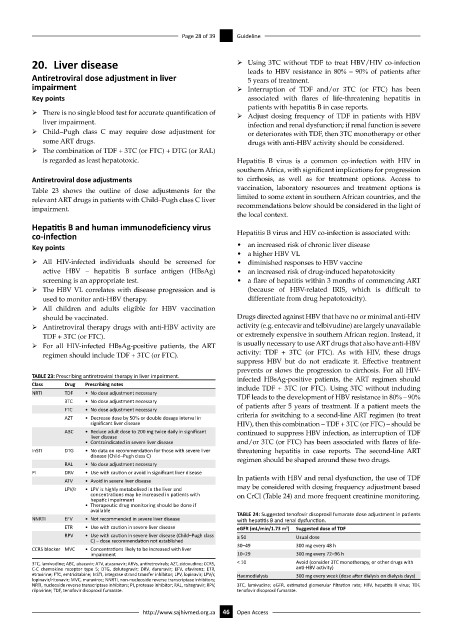
TABLE 23: Prescribing antiretroviral therapy in liver impairment. infected HBsAg-positive patients, the ART regimen should
Class Drug Prescribing notes include TDF + 3TC (or FTC). Using 3TC without including
NRTI TDF • No dose adjustment necessary TDF leads to the development of HBV resistance in 80% – 90%
3TC • No dose adjustment necessary
FTC • No dose adjustment necessary of patients after 5 years of treatment. If a patient meets the
AZT • Decrease dose by 50% or double dosage interval in criteria for switching to a second-line ART regimen (to treat
significant liver disease HIV), then this combination – TDF + 3TC (or FTC) – should be
ABC • Reduce adult dose to 200 mg twice daily in significant continued to suppress HBV infection, as interruption of TDF
liver disease
• Contraindicated in severe liver disease and/or 3TC (or FTC) has been associated with flares of life-
InSTI DTG • No data on recommendation for those with severe liver threatening hepatitis in case reports. The second-line ART
disease (Child–Pugh class C) regimen should be shaped around these two drugs.
RAL • No dose adjustment necessary
PI DRV • Use with caution or avoid in significant liver disease
ATV • Avoid in severe liver disease In patients with HBV and renal dysfunction, the use of TDF
LPV/r • LPV is highly metabolised in the liver and may be considered with dosing frequency adjustment based
concentrations may be increased in patients with on CrCl (Table 24) and more frequent creatinine monitoring.
hepatic impairment
• Therapeutic drug monitoring should be done if
available TABLE 24: Suggested tenofovir disoproxil fumarate dose adjustment in patients
NNRTI EFV • Not recommended in severe liver disease with hepatitis B and renal dysfunction.
ETR • Use with caution in severe liver disease eGFR (mL/min/1.73 m ) Suggested dose of TDF
2
RPV • Use with caution in severe liver disease (Child–Pugh class ≥ 50 Usual dose
C) – dose recommendation not established
CCR5 blocker MVC • Concentrations likely to be increased with liver 30–49 300 mg every 48 h
impairment 10–29 300 mg every 72–96 h
3TC, lamivudine; ABC, abacavir; ATV, atazanavir; ARVs, antiretrovirals; AZT, zidovudine; CCR5, < 10 Avoid (consider 3TC monotherapy, or other drugs with
C-C chemokine receptor type 5; DTG, dolutegravir; DRV, darunavir; EFV, efavirenz; ETR, anti-HBV activity)
etravirine; FTC, emtricitabine; InSTI, integrase strand transfer inhibitor; LPV, lopinavir; LPV/r, Haemodialysis 300 mg every week (dose after dialysis on dialysis days)
lopinavir/ritonavir; MVC, maraviroc; NNRTI, non-nucleoside reverse transcriptase inhibitors;
NRTI, nucleoside reverse transcriptase inhibitors; PI, protease inhibitor; RAL, raltegravir; RPV, 3TC, lamivudine; eGFR, estimated glomerular filtration rate; HBV, hepatitis B virus; TDF,
rilpivirine; TDF, tenofovir disoproxil fumarate. tenofovir disoproxil fumarate.
http://www.sajhivmed.org.za 46 Open Access