Page 52 - HIVMED_v21_i1.indb
P. 52
Page 26 of 39 Guideline
There is also uncertainty regarding the optimal dose of RFB ° Combining linezolid and AZT. These drugs should
with PI/r; these guidelines recommend 150 mg daily not be combined because both can cause bone marrow
(Table 20) for efficacy reasons, but careful monitoring for suppression (especially anaemia and neutropenia).
toxicity is required (ALT, neutrophil count and visual
symptoms at least monthly). RFB may be considered in 19. Pregnancy and breastfeeding
85
patients who are not able to tolerate co-treatment with
double-dose LPV/r and RIF-based TB treatment (i.e. Note: It is beyond the scope of these guidelines to provide
patients unable to tolerate the increased LPV/r dose comprehensive guidance for the management of pregnant
because of hepatotoxicity or GI side effects) or in ART- women. Key recommendations relating to the mother are
experienced patients on an ART regimen that is not included, but providers are encouraged to refer to national
guidelines. All women should be linked to routine antenatal
compatible with RIF (e.g. third-line ART with DRV/r). If care when pregnancy is confirmed.
RFB is unavailable and adjusted doses of LPV/r are poorly
tolerated in patients receiving second-line ART, then DTG • The prevention of mother-to-child transmission of HIV
(50 mg 12 hourly) may be substituted for the PI. However, (PMTCT) programme includes periconception, pregnancy,
it should be noted that good evidence is lacking regarding delivery and breastfeeding and encompasses the
the robustness of DTG in second-line therapy with both prevention of unplanned pregnancies.
NRTIs compromised, as exists for PI/r (section 13). • In low-resource settings, breastfeeding commonly
Nevertheless, the short-term use of DTG with two continues for up to 24 months. Breastfeeding transmission
compromised NRTIs over 6 months is preferable to treating is now the most common mode of mother-to-child
TB without RIF, which has a high risk of failure or relapse. transmission of HIV in many parts of sub-Saharan Africa,
rendering post-natal retention-in-care vital to successful
Antiretroviral therapy and TB medication share many side PMTCT intervention.
effects (Table 21). • Virological suppression on ART is essential for maternal
health, and to prevent HIV transmission to the infant. An
° Common pitfalls: elevated VL > 50 copies/mL in a pregnant or breastfeeding
° Rifampicin is co-administered with LPV/r, but woman requires urgent action.
the dose of LPV/r is not adjusted. This results • In well-functioning PMTCT programmes, a significant
in sub-therapeutic LPV concentrations and proportion of infections in infants result from undetected
development of PI resistance. Rifampicin should not seroconversion during pregnancy and breastfeeding.
be co-administered with ATV/r or DRV/r at all.
Repeated HIV testing throughout these periods is
essential for women initially testing HIV-negative.
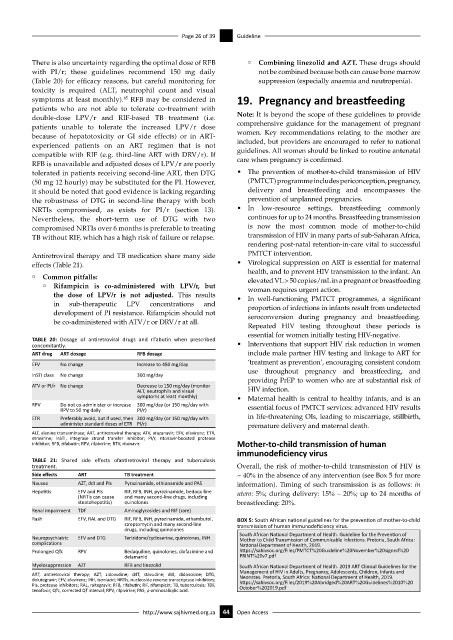
TABLE 20: Dosage of antiretroviral drugs and rifabutin when prescribed
concomitantly. • Interventions that support HIV risk reduction in women
ART drug ART dosage RFB dosage include male partner HIV testing and linkage to ART for
EFV No change Increase to 450 mg/day ‘treatment as prevention’, encouraging consistent condom
use throughout pregnancy and breastfeeding, and
InSTI class No change 300 mg/day
providing PrEP to women who are at substantial risk of
ATV or PI/r No change Decrease to 150 mg/day (monitor
ALT, neutrophils and visual HIV infection.
symptoms at least monthly) • Maternal health is central to healthy infants, and is an
RPV Do not co-administer or increase 300 mg/day (or 150 mg/day with essential focus of PMTCT services: advanced HIV results
RPV to 50 mg daily PI/r)
ETR Preferably avoid, but if used, then 300 mg/day (or 150 mg/day with in life-threatening OIs, leading to miscarriage, stillbirth,
administer standard doses of ETR PI/r) premature delivery and maternal death.
ALT, alanine transaminase; ART, antiretroviral therapy; ATV, atazanavir; EFV, efavirenz; ETR,
etravirine; InSTI, integrase strand transfer inhibitor; PI/r, ritonavir-boosted protease
inhibitor; RFB, rifabutin; RPV, rilpivirine; RTV, ritonavir. Mother-to-child transmission of human
immunodeficiency virus
TABLE 21: Shared side effects ofantiretroviral therapy and tuberculosis
treatment. Overall, the risk of mother-to-child transmission of HIV is
Side effects ART TB treatment ~ 40% in the absence of any intervention (see Box 5 for more
Nausea AZT, ddI and PIs Pyrazinamide, ethionamide and PAS information). Timing of such transmission is as follows: in
Hepatitis EFV and PIs RIF, RFB, INH, pyrazinamide, bedaquiline utero: 5%; during delivery: 15% – 20%; up to 24 months of
(NRTIs can cause and many second-line drugs, including
steatohepatitis) quinolones breastfeeding: 20%.
Renal impairment TDF Aminoglycosides and RIF (rare)
Rash EFV, RAL and DTG RIF, RFB, INH, pyrazinamide, ethambutol, BOX 5: South African national guidelines for the prevention of mother-to-child
streptomycin and many second-line transmission of human immunodeficiency virus.
drugs, including quinolones
South African National Department of Health. Guideline for the Prevention of
Neuropsychiatric EFV and DTG Terizidone/cycloserine, quinolones, INH Mother to Child Transmission of Communicable Infections. Pretoria, South Africa:
complications National Department of Health, 2019.
Prolonged QTc RPV Bedaquiline, quinolones, clofazimine and https://sahivsoc.org/Files/PMTCT%20Guideline%20November%20signed%20
delamanid PRINT%20v7.pdf
Myelosuppression AZT RFB and linezolid South African National Department of Health. 2019 ART Clinical Guidelines for the
ART, antiretroviral therapy; AZT, zidovudine; d4T, stavudine; ddI, didanosine; DTG, Management of HIV in Adults, Pregnancy, Adolescents, Children, Infants and
dolutegravir; EFV, efavirenz; INH, isoniazid; NRTIs, nucleoside reverse transcriptase inhibitors; Neonates. Pretoria, South Africa: National Department of Health, 2019.
PIs, protease inhibitors; RAL, raltegravir; RFB, rifabutin; RIF, rifampicin; TB, tuberculosis; TDF, https://sahivsoc.org/Files/2019%20Abridged%20ART%20Guidelines%2010%20
tenofovir; QTc, corrected QT interval; RPV, rilpivirine; PAS, p-aminosalicylic acid. October%202019.pdf
http://www.sajhivmed.org.za 44 Open Access