Page 53 - HIVMED_v21_i1.indb
P. 53
Page 27 of 39 Guideline
The time of the highest risk coincides with delivery, which • Dose adjustment of ART during pregnancy is only
spans a matter of hours; the risk during 24 months of indicated for women taking both TDF and ATV/r during
breastfeeding is slightly higher, but over a significantly the second/third trimester; the dose should be increased
greater timespan. Breastfeeding should not be stopped from ATV/r 300 mg/100 mg to 400 mg/100 mg.
because of a new diagnosis of HIV, or an elevated VL in • Women taking LPV/r 800 mg/200 mg daily should be
women already on ART. Instead, initiation of ART and advised to adjust this to 400 mg/100 mg 12 hourly
management of raised VL (together with infant prophylaxis) (twice daily) during pregnancy because of altered
are interventions to ‘make breastfeeding safer’. pharmacokinetics. These women should also be informed
about the association between LPV/r and premature
Antiretroviral therapy for women of labour and delivery.
childbearing potential and during pregnancy • Particular importance should be placed on drug–drug
and breastfeeding interactions between DTG and divalent cation-containing
medication in pregnancy, as pregnant women frequently
All HIV-positive pregnant and breastfeeding women
should be initiated on lifelong ART, ideally the same day receive iron supplements and/or magnesium-/aluminium-
containing antacids.
that pregnancy is confirmed. Standard first-, second- and
third-line regimens should be used in pregnancy (see the Patients returning to care in pregnancy after defaulting a
sections ‘Initial antiretroviral therapy regimens for the first-line regimen or those exposed to previous PMTCT
previously untreated patient’, ‘Management of patients regimens should generally be put directly on a DTG-based
currently receiving first-line therapy’, ‘Management of regimen, rather than retrying an NNRTI-regimen
patients starting or currently receiving second-line therapy’ (section 16). As per current PMTCT guidelines, women not
and ‘Third-line antiretroviral therapy’). Regarding DTG already on ART at the time of labour or delivery should
use in pregnancy, it is important to note that the commence TLD immediately and also receive an additional
absolute risk of NTD is low (< 0.5%), and this risk may be stat dose of NVP 200 mg. Women who are newly diagnosed
outweighed by the additional benefits of DTG over with HIV during the breastfeeding period may continue
alternative therapies. We currently recommend that WOCP breastfeeding as per maternal preference, provided that
who wish to become pregnant or who have no reliable maternal ART and infant prophylaxis are initiated and
access to effective contraception should be counselled adherence support is given.
adequately about the potential risks and benefits of
DTG- versus EFV-based ART, and should be offered the Other key recommendations:
choice of first-line regimens. • All pregnant women should be screened at every visit for
sexually transmitted infections and treated as needed.
Other points regarding ART in pregnancy include the • All pregnant and breastfeeding women should be
following: screened for TB at every visit. If the TB screening
is negative, then consider TB-preventive therapy
• Efavirenz 600 mg is a safe and effective regimen for use +
by WOCP including during the time from conception to during pregnancy only in women with a CD4 count
< 350 cells/μL (section 27).
the end of the first trimester. There are insufficient data to
recommend routine use of EFV 400 mg in pregnant
° Common pitfalls:
women.
° Not performing VL monitoring at appropriate
• The current guidelines no longer recommend initiating time. See Table 22 for the appropriate monitoring
NVP in any patients. Maternal deaths in pregnant women intervals.
have been associated with NVP because of liver and skin ° An elevated VL is not acted upon urgently. Viral load
hypersensitivity reactions. results should be fast-tracked, and women failing
• NRTIs: Note that commonly used CrCl calculations are their current regimen must be identified early and, if
not validated for pregnant women; therefore, avoid TDF necessary, a regimen switch should be made without
if serum Cr ≥ 85 μmol/L. delay.
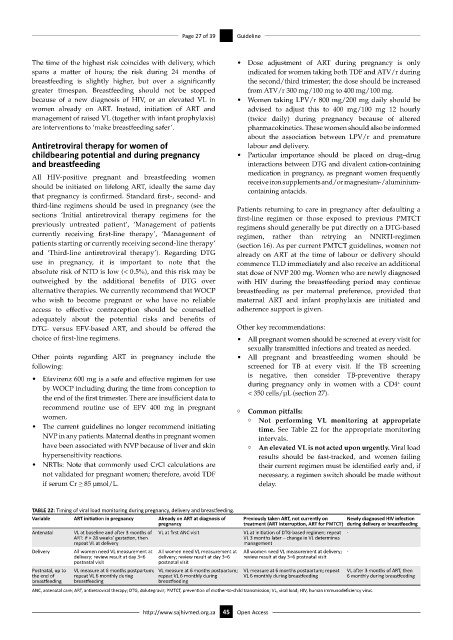
TABLE 22: Timing of viral load monitoring during pregnancy, delivery and breastfeeding.
Variable ART initiation in pregnancy Already on ART at diagnosis of Previously taken ART, not currently on Newly diagnosed HIV infection
pregnancy treatment (ART interruption, ART for PMTCT) during delivery or breastfeeding
Antenatal VL at baseline and after 3 months of VL at first ANC visit VL at initiation of DTG-based regimen; repeat -
ART: if > 28 weeks’ gestation, then VL 3 months later – change in VL determines
repeat VL at delivery management
Delivery All women need VL measurement at All women need VL measurement at All women need VL measurement at delivery; -
delivery; review result at day 3–6 delivery; review result at day 3–6 review result at day 3–6 postnatal visit
postnatal visit postnatal visit
Postnatal, up to VL measure at 6 months postpartum; VL measure at 6 months postpartum; VL measure at 6 months postpartum; repeat VL after 3 months of ART, then
the end of repeat VL 6 monthly during repeat VL 6 monthly during VL 6 monthly during breastfeeding 6 monthly during breastfeeding
breastfeeding breastfeeding breastfeeding
ANC, antenatal care; ART, antiretroviral therapy; DTG, dolutegravir; PMTCT, prevention of mother-to-child transmission; VL, viral load; HIV, human immunodeficiency virus.
http://www.sajhivmed.org.za 45 Open Access