Page 218 - SAHCS HIVMed Journal Vol 20 No 1 2019
P. 218
Page 6 of 7 Original Research
intracranial saccular aneurysms in HIV infection is majority of cases. The presence of unilateral or bilateral
unsubstantiated; however, dolichoectatic vessels from enhancing masses did not provide any clues to the underlying
11
immune-mediated vessel damage are more plausible. In this pathology. However, MRI was diagnostic in the case of the
first case series of cavernous sinus disease in HIV-coinfected pituitary adenoma and saccular internal carotid artery
patients, we describe HIV- and non-HIV-related pathology. disease, which, in all probability, were incidental disorders.
The third cranial nerve was the commonest cranial nerve CSF findings were positive in confirming the diagnosis in 31%
affected in this group followed by involvement of the sixth (4/13) of the patients, which included one patient with TB, one
cranial nerve, the ophthalmic division of the fifth cranial nerve patient with cryptococcal meningitis and two patients with
and then the fourth cranial nerve. Unlike the third and sixth neurosyphilis. While treatment at the tertiary centre was
cranial nerve palsies, the fourth nerve palsy did not occur in appropriately initiated, continuation and follow-up care was
isolation. The Horner syndrome was present in one patient only. poor. It is not unusual for patients to ‘disappear’ into a void or
This could imply a rare occurrence or difficulty in detection in be lost in the system after discharge from the tertiary centre. In
the presence of other cranial nerve palsies. Unilateral disease most instances, the fault lies with the highly prohibitive referral
was present in 65% of the patients despite the connection of the system to tertiary and academic centres in South Africa. The
two cavernous sinuses by the circular sinus. Proptosis and visual apathy and lack of social support are other contributing factors.
impairment were uncommon implying minimal extension of
pathology from the cavernous sinus to the orbital apex. This study was a retrospective chart review and hence
fraught with many limitations as evidenced by a deficiency
The magnetic resonance imaging and computed tomography of appropriate and detailed record-keeping. Furthermore,
findings of cavernous sinus disease were helpful in localising the follow-up of patients was poor, especially when referred
the disorder but not in elucidating the pathology in the to other departments for co-management.
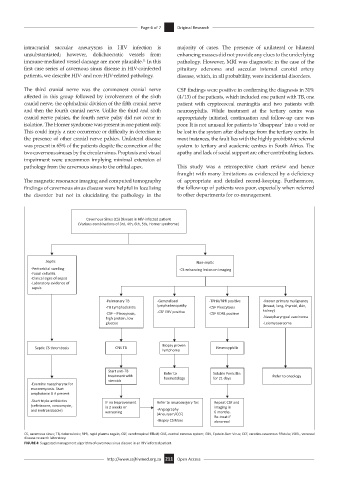
Cavernous Sinus (CS) Disease in HIV-infected pa ent
(Various combina ons of 3rd, 4th, 6th, 5th, Horner syndrome)
Sep c Non-sep c
-Peri-orbital swelling -CS enhancing lesion on imaging
-Facial celluli s
-Clinical signs of sepsis
-Laboratory evidence of
sepsis
-Pulmonary TB -Generalised -TPHA/RPR posi ve -Known primary malignancy
-TB Lymphadeni s lymphadenopathy -CSF Pleocytosis (breast, lung, thyroid, skin,
-CSF – Pleocytosis, -CSF EBV posi ve -CSF VDRL posi ve kidney)
high protein, low -Nasopharyngeal carcinoma
glucose -Leiomyosarcoma
Biopsy proven
Sep c CS thrombosis CNS TB Neurosyphilis
lymphoma
Start an -TB Refer to Soluble Penicillin
treatment with haematology for 21 days Refer to oncology
steroids
-Examine nasopharynx for
mucormycosis. Start
amphoterin B if present
-Start triple an bio cs IF no Improvement Refer to neurosurgery for: Repeat CSF and
(ceriaxone, vancomycin, in 2 weeks or imaging in
and metronidazole) worsening -Angiography 6 months.
(Aneurysm/CCF) Re-treat if
-Biopsy CS Mass abnormal
CS, cavernous sinus; TB, tuberculosis; RPR, rapid plasma regain; CSF, cerebrospinal flfluid; CNS, central nervous system; EBV, Epstein-Barr Virus; CCF, carotico-cavernous fifistula; VDRL, venereal
disease research laboratory.
FIGURE 4: Suggested management algorithm of cavernous sinus disease in an HIV-infected patient.
http://www.sajhivmed.org.za 211 Open Access