Page 36 - HIVMED_v21_i1.indb
P. 36
Page 10 of 39 Guideline
42
inflammation that may drive non-infectious morbidities. Medical reasons to delay antiretroviral therapy initiation
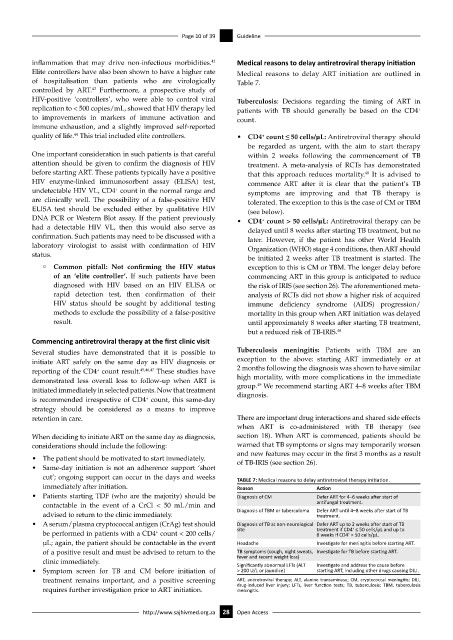
Elite controllers have also been shown to have a higher rate Medical reasons to delay ART initiation are outlined in
of hospitalisation than patients who are virologically Table 7.
43
controlled by ART. Furthermore, a prospective study of
HIV-positive ‘controllers’, who were able to control viral Tuberculosis: Decisions regarding the timing of ART in
replication to < 500 copies/mL, showed that HIV therapy led patients with TB should generally be based on the CD4
+
to improvements in markers of immune activation and count.
immune exhaustion, and a slightly improved self-reported
44
quality of life. This trial included elite controllers. • CD4 count ≤ 50 cells/µL: Antiretroviral therapy should
+
be regarded as urgent, with the aim to start therapy
One important consideration in such patients is that careful within 2 weeks following the commencement of TB
attention should be given to confirm the diagnosis of HIV treatment. A meta-analysis of RCTs has demonstrated
before starting ART. These patients typically have a positive that this approach reduces mortality. It is advised to
48
HIV enzyme-linked immunosorbent assay (ELISA) test, commence ART after it is clear that the patient’s TB
+
undetectable HIV VL, CD4 count in the normal range and symptoms are improving and that TB therapy is
are clinically well. The possibility of a false-positive HIV tolerated. The exception to this is the case of CM or TBM
ELISA test should be excluded either by qualitative HIV (see below).
DNA PCR or Western Blot assay. If the patient previously • CD4 count > 50 cells/µL: Antiretroviral therapy can be
+
had a detectable HIV VL, then this would also serve as delayed until 8 weeks after starting TB treatment, but no
confirmation. Such patients may need to be discussed with a later. However, if the patient has other World Health
laboratory virologist to assist with confirmation of HIV Organization (WHO) stage 4 conditions, then ART should
status.
be initiated 2 weeks after TB treatment is started. The
° Common pitfall: Not confirming the HIV status exception to this is CM or TBM. The longer delay before
of an ‘elite controller’. If such patients have been commencing ART in this group is anticipated to reduce
diagnosed with HIV based on an HIV ELISA or the risk of IRIS (see section 26). The aforementioned meta-
rapid detection test, then confirmation of their analysis of RCTs did not show a higher risk of acquired
HIV status should be sought by additional testing immune deficiency syndrome (AIDS) progression/
methods to exclude the possibility of a false-positive mortality in this group when ART initiation was delayed
result. until approximately 8 weeks after starting TB treatment,
but a reduced risk of TB-IRIS. 48
Commencing antiretroviral therapy at the first clinic visit
Several studies have demonstrated that it is possible to Tuberculosis meningitis: Patients with TBM are an
initiate ART safely on the same day as HIV diagnosis or exception to the above: starting ART immediately or at
reporting of the CD4 count result. 45,46,47 These studies have 2 months following the diagnosis was shown to have similar
+
demonstrated less overall loss to follow-up when ART is high mortality, with more complications in the immediate
49
initiated immediately in selected patients. Now that treatment group. We recommend starting ART 4–8 weeks after TBM
diagnosis.
is recommended irrespective of CD4 count, this same-day
+
strategy should be considered as a means to improve
retention in care. There are important drug interactions and shared side effects
when ART is co-administered with TB therapy (see
When deciding to initiate ART on the same day as diagnosis, section 18). When ART is commenced, patients should be
considerations should include the following: warned that TB symptoms or signs may temporarily worsen
and new features may occur in the first 3 months as a result
• The patient should be motivated to start immediately. of TB-IRIS (see section 26).
• Same-day initiation is not an adherence support ‘short
cut’; ongoing support can occur in the days and weeks TABLE 7: Medical reasons to delay antiretroviral therapy initiation.
immediately after initiation. Reason Action
• Patients starting TDF (who are the majority) should be Diagnosis of CM Defer ART for 4–6 weeks after start of
contactable in the event of a CrCl < 50 mL/min and antifungal treatment.
advised to return to the clinic immediately. Diagnosis of TBM or tuberculoma Defer ART until 4–8 weeks after start of TB
treatment.
• A serum/plasma cryptococcal antigen (CrAg) test should Diagnosis of TB at non-neurological Defer ART up to 2 weeks after start of TB
+
be performed in patients with a CD4 count < 200 cells/ site treatment if CD4 ≤ 50 cells/µL and up to
+
+
8 weeks if CD4 > 50 cells/µL.
μL; again, the patient should be contactable in the event Headache Investigate for meningitis before starting ART.
of a positive result and must be advised to return to the TB symptoms (cough, night sweats, Investigate for TB before starting ART.
fever and recent weight loss)
clinic immediately. Significantly abnormal LFTs (ALT Investigate and address the cause before
• Symptom screen for TB and CM before initiation of > 200 U/L or jaundice) starting ART, including other drugs causing DILI.
treatment remains important, and a positive screening ART, antiretroviral therapy; ALT, alanine transaminase; CM, cryptococcal meningitis; DILI,
requires further investigation prior to ART initiation. drug-induced liver injury; LFTs, liver function tests; TB, tuberculosis; TBM, tuberculosis
meningitis.
http://www.sajhivmed.org.za 28 Open Access