Page 431 - HIVMED_v21_i1.indb
P. 431
Page 4 of 7 Original Research
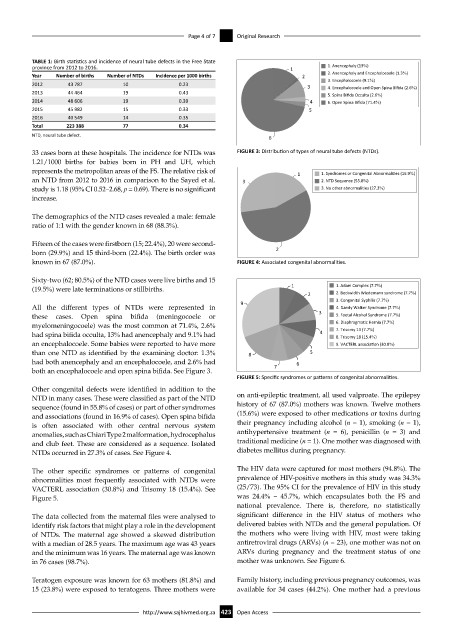
TABLE 1: Birth statistics and incidence of neural tube defects in the Free State
province from 2012 to 2016. 1 1. Anencephaly (13%)
Year Number of births Number of NTDs Incidence per 1000 births 2 2. Anencephaly and Encephalocoele (1.3%)
2012 43 787 10 0.23 3 3. Encephalocoele (9.1%)
4. Encephalocoele and Open Spina Bifida (2.6%)
2013 44 464 19 0.43 5. Spina Bifida Occulta (2.6%)
2014 48 606 19 0.39 4 6. Open Spina Bifida (71.4%)
2015 45 982 15 0.33 5
2016 40 549 14 0.35
Total 223 388 77 0.34
NTD, neural tube defect. 6
33 cases born at these hospitals. The incidence for NTDs was FIGURE 3: Distribution of types of neural tube defects (NTDs).
1.21/1000 births for babies born in PH and UH, which
represents the metropolitan areas of the FS. The relative risk of 1 1. Syndromes or Congenital Abnormali es (16.9%)
an NTD from 2012 to 2016 in comparison to the Sayed et al. 3 2. NTD Sequence (55.8%)
study is 1.18 (95% CI 0.52–2.68, p = 0.69). There is no significant 3. No other abnormali es (27.3%)
increase.
The demographics of the NTD cases revealed a male: female
ratio of 1:1 with the gender known in 68 (88.3%).
Fifteen of the cases were firstborn (15; 22.4%), 20 were second-
born (29.9%) and 15 third-born (22.4%). The birth order was 2
known in 67 (87.0%). FIGURE 4: Associated congenital abnormalities.
Sixty-two (62; 80.5%) of the NTD cases were live births and 15
(19.5%) were late terminations or stillbirths. 1 1. Adam Complex (7.7%)
2 2. Beckwidth Wiedemann syndrome (7.7%)
9 3. Congenital Syphilis (7.7%)
All the different types of NTDs were represented in 4. Dandy Walker Syndrome (7.7%)
these cases. Open spina bifida (meningocoele or 3 5. Foetal Alcohol Syndrome (7.7%)
myelomeningocoele) was the most common at 71.4%, 2.6% 6. Diaphragma c Hernia (7.7%)
7. Trisomy 13 (7.7%)
had spina bifida occulta, 13% had anencephaly and 9.1% had 4 8. Trisomy 18 (15.4%)
an encephalocoele. Some babies were reported to have more 9. VACTERL associa on (30.8%)
than one NTD as identified by the examining doctor: 1.3% 8 5
had both anencephaly and an encephalocoele, and 2.6% had 6
both an encephalocoele and open spina bifida. See Figure 3. 7
FIGURE 5: Specific syndromes or patterns of congenital abnormalities.
Other congenital defects were identified in addition to the
NTD in many cases. These were classified as part of the NTD on anti-epileptic treatment, all used valproate. The epilepsy
sequence (found in 55.8% of cases) or part of other syndromes history of 67 (87.0%) mothers was known. Twelve mothers
and associations (found in 16.9% of cases). Open spina bifida (15.6%) were exposed to other medications or toxins during
is often associated with other central nervous system their pregnancy including alcohol (n = 1), smoking (n = 1),
anomalies, such as Chiari Type 2 malformation, hydrocephalus antihypertensive treatment (n = 6), penicillin (n = 3) and
and club feet. These are considered as a sequence. Isolated traditional medicine (n = 1). One mother was diagnosed with
NTDs occurred in 27.3% of cases. See Figure 4. diabetes mellitus during pregnancy.
The other specific syndromes or patterns of congenital The HIV data were captured for most mothers (94.8%). The
abnormalities most frequently associated with NTDs were prevalence of HIV-positive mothers in this study was 34.3%
VACTERL association (30.8%) and Trisomy 18 (15.4%). See (25/73). The 95% CI for the prevalence of HIV in this study
Figure 5. was 24.4% – 45.7%, which encapsulates both the FS and
national prevalence. There is, therefore, no statistically
The data collected from the maternal files were analysed to significant difference in the HIV status of mothers who
identify risk factors that might play a role in the development delivered babies with NTDs and the general population. Of
of NTDs. The maternal age showed a skewed distribution the mothers who were living with HIV, most were taking
with a median of 28.5 years. The maximum age was 43 years antiretroviral drugs (ARVs) (n = 23), one mother was not on
and the minimum was 16 years. The maternal age was known ARVs during pregnancy and the treatment status of one
in 76 cases (98.7%). mother was unknown. See Figure 6.
Teratogen exposure was known for 63 mothers (81.8%) and Family history, including previous pregnancy outcomes, was
15 (23.8%) were exposed to teratogens. Three mothers were available for 34 cases (44.2%). One mother had a previous
http://www.sajhivmed.org.za 423 Open Access