Page 432 - HIVMED_v21_i1.indb
P. 432
Page 5 of 7 Original Research
The referrals from outside UH were classified according to
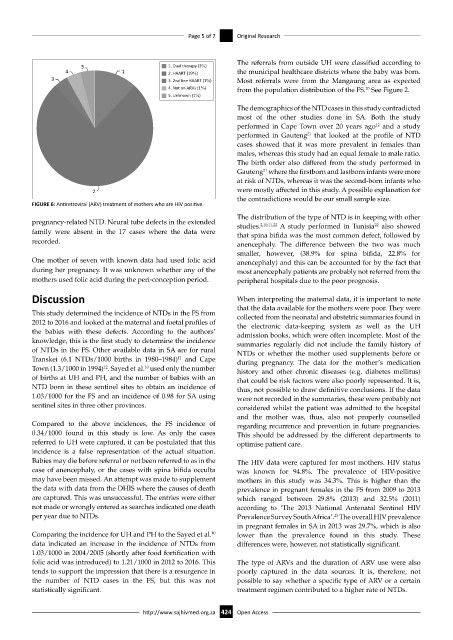
5 1. Dual therapy (3%)
4 1 2. HAART (19%) the municipal healthcare districts where the baby was born.
3 3. 2nd line HAART (1%) Most referrals were from the Mangaung area as expected
4. Not on ARVs (1%) from the population distribution of the FS. See Figure 2.
20
5. Unknown (1%)
The demographics of the NTD cases in this study contradicted
most of the other studies done in SA. Both the study
performed in Cape Town over 20 years ago and a study
12
performed in Gauteng that looked at the profile of NTD
21
cases showed that it was more prevalent in females than
males, whereas this study had an equal female to male ratio.
The birth order also differed from the study performed in
Gauteng where the firstborn and lastborn infants were more
21
at risk of NTDs, whereas it was the second-born infants who
2 were mostly affected in this study. A possible explanation for
the contradictions would be our small sample size.
FIGURE 6: Antiretroviral (ARV) treatment of mothers who are HIV positive.
The distribution of the type of NTD is in keeping with other
pregnancy-related NTD. Neural tube defects in the extended studies. 2,10,11,22 A study performed in Tunisia also showed
22
family were absent in the 17 cases where the data were that spina bifida was the most common defect, followed by
recorded. anencephaly. The difference between the two was much
smaller, however, (38.9% for spina bifida, 22.8% for
One mother of seven with known data had used folic acid anencephaly) and this can be accounted for by the fact that
during her pregnancy. It was unknown whether any of the most anencephaly patients are probably not referred from the
mothers used folic acid during the peri-conception period. peripheral hospitals due to the poor prognosis.
Discussion When interpreting the maternal data, it is important to note
that the data available for the mothers were poor. They were
This study determined the incidence of NTDs in the FS from collected from the neonatal and obstetric summaries found in
2012 to 2016 and looked at the maternal and foetal profiles of the electronic data-keeping system as well as the UH
the babies with these defects. According to the authors’ admission books, which were often incomplete. Most of the
knowledge, this is the first study to determine the incidence summaries regularly did not include the family history of
of NTDs in the FS. Other available data in SA are for rural NTDs or whether the mother used supplements before or
Transkei (6.1 NTDs/1000 births in 1980–1984) and Cape during pregnancy. The data for the mother’s medication
11
Town (1.3/1000 in 1994) . Sayed et al. used only the number history and other chronic diseases (e.g. diabetes mellitus)
10
12
of births at UH and PH, and the number of babies with an that could be risk factors were also poorly represented. It is,
NTD born in these sentinel sites to obtain an incidence of thus, not possible to draw definitive conclusions. If the data
1.03/1000 for the FS and an incidence of 0.98 for SA using were not recorded in the summaries, these were probably not
sentinel sites in three other provinces. considered whilst the patient was admitted to the hospital
and the mother was, thus, also not properly counselled
Compared to the above incidences, the FS incidence of regarding recurrence and prevention in future pregnancies.
0.34/1000 found in this study is low. As only the cases This should be addressed by the different departments to
referred to UH were captured, it can be postulated that this optimise patient care.
incidence is a false representation of the actual situation.
Babies may die before referral or not been referred to as in the The HIV data were captured for most mothers. HIV status
case of anencephaly, or the cases with spina bifida occulta was known for 94.8%. The prevalence of HIV-positive
may have been missed. An attempt was made to supplement mothers in this study was 34.3%. This is higher than the
the data with data from the DHIS where the causes of death prevalence in pregnant females in the FS from 2009 to 2013
are captured. This was unsuccessful. The entries were either which ranged between 29.8% (2013) and 32.5% (2011)
not made or wrongly entered as searches indicated one death according to ‘The 2013 National Antenatal Sentinel HIV
per year due to NTDs. Prevalence Survey South Africa’. The overall HIV prevalence
23
in pregnant females in SA in 2013 was 29.7%, which is also
Comparing the incidence for UH and PH to the Sayed et al. lower than the prevalence found in this study. These
10
data indicated an increase in the incidence of NTDs from differences were, however, not statistically significant.
1.03/1000 in 2004/2005 (shortly after food fortification with
folic acid was introduced) to 1.21/1000 in 2012 to 2016. This The type of ARVs and the duration of ARV use were also
tends to support the impression that there is a resurgence in poorly captured in the data sources. It is, therefore, not
the number of NTD cases in the FS, but this was not possible to say whether a specific type of ARV or a certain
statistically significant. treatment regimen contributed to a higher rate of NTDs.
http://www.sajhivmed.org.za 424 Open Access