Page 168 - HIVMED_v21_i1.indb
P. 168
Page 6 of 8 Original Research
120 < 10 ng/mL 10–100 ng/mL > 100 mg/ml a 120 < 10 ng/mL 10–100 ng/mL > 100 mg/ml b
100 100
23.2 24.1 29.6 80 25 25
80
Propor on (%) 60 15.6 15.5 13.6 Propor on (%) 60 15 14
40
62.3 61.4 56.8 40 60 61
20 20
0 0 0 0 0
< = 34 35–44 45–54 > = 55 Men Women
Age groups in years (p = 0.724) Gender (p = 0.940)
120 < 10 ng/mL 10–100 ng/mL > 100 mg/ml c 120 < 10 ng/mL 10–100 ng/mL > 100 mg/ml d
100 100
26 23 80 26 21
80
Propor on (%) 60 14 14 Propor on (%) 60 14 14
40
60 63 40 60 65
20 20
0 0
< 5 years > = 5 years < 396/mm 3 > = 396/mm 3
Diagnosed dura on of HIV (p = 0.681) CD4 count (p = 0.505)
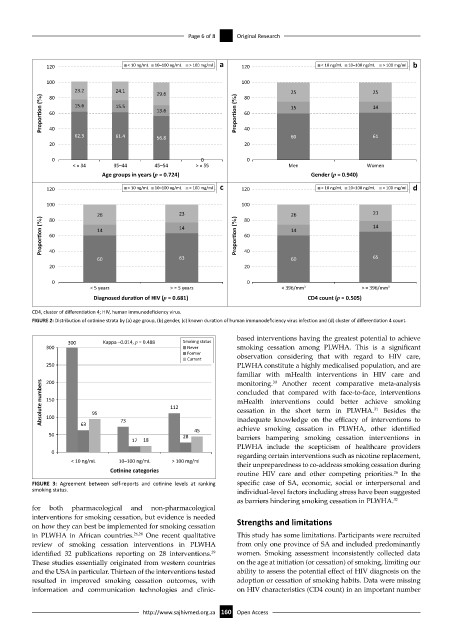
CD4, cluster of differentiation 4; HIV, human immunodeficiency virus.
FIGURE 2: Distribution of cotinine strata by (a) age group, (b) gender, (c) known duration of human immunodeficiency virus infection and (d) cluster of differentiation 4 count.
based interventions having the greatest potential to achieve
300 Kappa –0.014, p = 0.488 Smoking status
300 Never smoking cessation among PLWHA. This is a significant
Former observation considering that with regard to HIV care,
Current
250 PLWHA constitute a highly medicalised population, and are
familiar with mHealth interventions in HIV care and
200
Absolute numbers 150 95 112 concluded that compared with face-to-face, interventions
monitoring. Another recent comparative meta-analysis
30
mHealth interventions could better achieve smoking
31
cessation in the short term in PLWHA. Besides the
100
73
63
achieve smoking cessation in PLWHA, other identified
45 inadequate knowledge on the efficacy of interventions to
50 28 barriers hampering smoking cessation interventions in
17 18
PLWHA include the scepticism of healthcare providers
0 regarding certain interventions such as nicotine replacement,
< 10 ng/mL 10–100 ng/mL > 100 mg/ml their unpreparedness to co-address smoking cessation during
Co nine categories
26
routine HIV care and other competing priorities. In the
FIGURE 3: Agreement between self-reports and cotinine levels at ranking specific case of SA, economic, social or interpersonal and
smoking status. individual-level factors including stress have been suggested
as barriers hindering smoking cessation in PLWHA. 32
for both pharmacological and non-pharmacological
interventions for smoking cessation, but evidence is needed
on how they can best be implemented for smoking cessation Strengths and limitations
in PLWHA in African countries. 26,28 One recent qualitative This study has some limitations. Participants were recruited
review of smoking cessation interventions in PLWHA from only one province of SA and included predominantly
identified 32 publications reporting on 28 interventions. women. Smoking assessment inconsistently collected data
29
These studies essentially originated from western countries on the age at initiation (or cessation) of smoking, limiting our
and the USA in particular. Thirteen of the interventions tested ability to assess the potential effect of HIV diagnosis on the
resulted in improved smoking cessation outcomes, with adoption or cessation of smoking habits. Data were missing
information and communication technologies and clinic- on HIV characteristics (CD4 count) in an important number
http://www.sajhivmed.org.za 160 Open Access