Page 120 - HIVMED_v21_i1.indb
P. 120
Page 29 of 34 Guideline
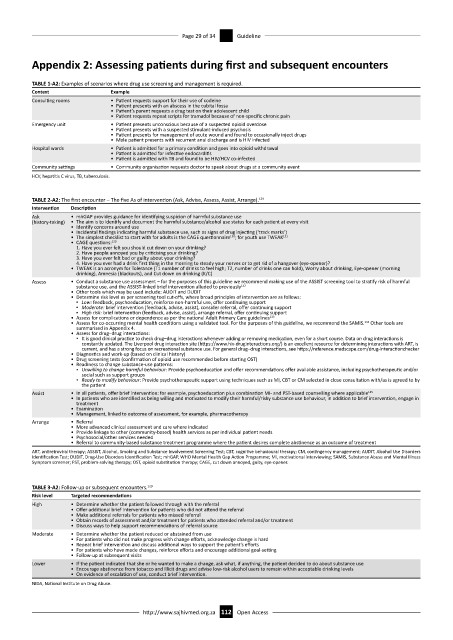
Appendix 2: Assessing patients during first and subsequent encounters
TABLE 1-A2: Examples of scenarios where drug use screening and management is required.
Context Example
Consulting rooms • Patient requests support for their use of codeine
• Patient presents with an abscess in the cubital fossa
• Patient’s parent requests a drug test on their adolescent child
• Patient requests repeat scripts for tramadol because of non-specific chronic pain
Emergency unit • Patient presents unconscious because of a suspected opioid overdose
• Patient presents with a suspected stimulant-induced psychosis
• Patient presents for management of acute wound and found to occasionally inject drugs
• Male patient presents with recurrent anal discharge and is HIV infected
Hospital wards • Patient is admitted for a primary condition and goes into opioid withdrawal
• Patient is admitted for infective endocarditis
• Patient is admitted with TB and found to be HIV/HCV co-infected
Community settings • Community organisation requests doctor to speak about drugs at a community event
HCV, hepatitis C virus, TB, tuberculosis.
TABLE 2-A2: The first encounter – The five As of intervention (Ask, Advise, Assess, Assist, Arrange). 129
Intervention Description
Ask • mhGAP provides guidance for identifying suspicion of harmful substance use
(history-taking) • The aim is to identify and document the harmful substance/alcohol use status for each patient at every visit
• Identify concerns around use
• Incidental findings indicating harmful substance use, such as signs of drug injecting (‘track marks’)
• The simplest checklist to start with for adults is the CAGE questionnaire ; for youth use TWEAK 131
130
• CAGE questions: 130
1. Have you ever felt you should cut down on your drinking?
2. Have people annoyed you by criticising your drinking?
3. Have you ever felt bad or guilty about your drinking?
4. Have you ever had a drink first thing in the morning to steady your nerves or to get rid of a hangover (eye-opener)?
• TWEAK is an acronym for Tolerance (T1 number of drinks to feel high; T2, number of drinks one can hold), Worry about drinking, Eye-opener (morning
drinking), Amnesia (blackouts), and Cut down on drinking (K/C)
Assess • Conduct a substance use assessment – for the purposes of this guideline we recommend making use of the ASSIST screening tool to stratify risk of harmful
substance use, and the ASSIST-linked brief intervention alluded to previously 132
• Other tools which may be used include: AUDIT and DUDIT
• Determine risk level as per screening tool cut-offs, where broad principles of intervention are as follows:
▪ Low: feedback, psychoeducation, reinforce non-harmful use, offer continuing support
▪ Moderate: brief intervention (feedback, advise, assist), consider referral, offer continuing support
▪ High risk: brief intervention (feedback, advise, assist), arrange referral, offer continuing support
• Assess for complications or dependence as per the national Adult Primary Care guidelines 133
• Assess for co-occurring mental health conditions using a validated tool. For the purposes of this guideline, we recommend the SAMIS. Other tools are
134
summarised in Appendix 4.
• Assess for drug–drug interactions:
▪ It is good clinical practice to check drug–drug interactions whenever adding or removing medication, even for a short course. Data on drug interactions is
constantly updated. The Liverpool drug interaction site (https://www.hiv-druginteractions.org/) is an excellent resource for determining interactions with ART, is
current, and has a strong focus on recreational substance use. For general drug–drug interactions, see https://reference.medscape.com/drug-interactionchecker
• Diagnostics and work-up (based on clinical history)
• Drug screening tests (confirmation of opioid use recommended before starting OST)
• Readiness to change substance-use patterns:
▪ Unwilling to change harmful behaviour: Provide psychoeducation and offer recommendations offer available assistance, including psychotherapeutic and/or
social such as support groups
▪ Ready to modify behaviour: Provide psychotherapeutic support using techniques such as MI, CBT or CM selected in close consultation with/as is agreed to by
the patient
Assist • In all patients, offer brief intervention: for example, psychoeducation plus combination MI- and PST-based counselling where applicable 135
• In patients who are identified as being willing and motivated to modify their harmful/risky substance use behaviour, in addition to brief intervention, engage in
treatment
• Examination
• Management, linked to outcome of assessment, for example, pharmacotherapy
Arrange • Referral
• More advanced clinical assessment and care where indicated
• Provide linkage to other (community-based) health services as per individual patient needs
• Psychosocial/other services needed
• Referral to community-based substance treatment programme where the patient desires complete abstinence as an outcome of treatment
ART, antiretroviral therapy; ASSIST, Alcohol, Smoking and Substance Involvement Screening Test; CBT, cognitive behavioural therapy; CM, contingency management; AUDIT, Alcohol Use Disorders
Identification Test; DUDIT, Drug-Use Disorders Identification Test; mhGAP, WHO Mental Health Gap Action Programme; MI, motivational interviewing; SAMIS, Substance Abuse and Mental Illness
Symptom screener; PST, problem-solving therapy; OST, opioid substitution therapy; CAGE, cut down annoyed, guity, eye-opener.
TABLE 3-A2: Follow-up or subsequent encounters. 129
Risk level Targeted recommendations
High • Determine whether the patient followed through with the referral
• Offer additional brief intervention for patients who did not attend the referral
• Make additional referrals for patients who missed referral
• Obtain records of assessment and/or treatment for patients who attended referral and/or treatment
• Discuss ways to help support recommendations of referral source
Moderate • Determine whether the patient reduced or abstained from use
• For patients who did not make progress with change efforts, acknowledge change is hard
• Repeat brief intervention and discuss additional ways to support the patient’s efforts
• For patients who have made changes, reinforce efforts and encourage additional goal-setting
• Follow-up at subsequent visits
Lower • If the patient indicated that she or he wanted to make a change, ask what, if anything, the patient decided to do about substance use
• Encourage abstinence from tobacco and illicit drugs and advise low-risk alcohol users to remain within acceptable drinking levels
• On evidence of escalation of use, conduct brief intervention.
NIDA, National Institute on Drug Abuse.
http://www.sajhivmed.org.za 112 Open Access