Page 121 - HIVMED_v21_i1.indb
P. 121
Page 30 of 34 Guideline
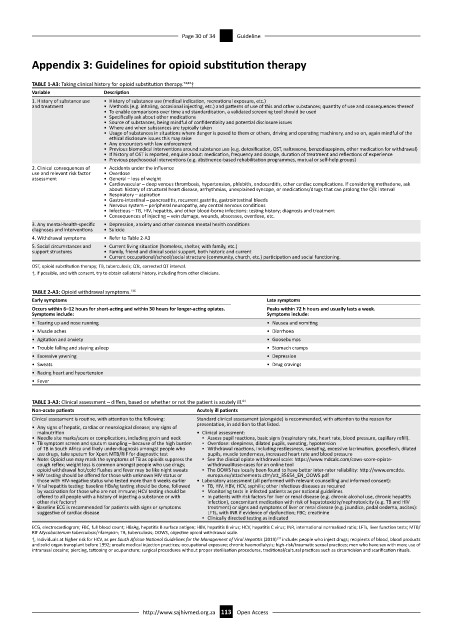
Appendix 3: Guidelines for opioid substitution therapy
TABLE 1-A3: Taking clinical history for opioid substitution therapy. 74,83 †
Variable Description
1. History of substance use • History of substance use (medical indication, recreational exposure, etc.)
and treatment • Methods (e.g. inhaling, occasional injecting, etc.) and patterns of use of this and other substances; quantity of use and consequences thereof
• To enable comparisons over time and standardisation, a validated screening tool should be used
• Specifically ask about other medications
• Source of substances, being mindful of confidentiality and potential disclosure issues
• Where and when substances are typically taken
• Usage of substances in situations where danger is posed to them or others, driving and operating machinery, and so on, again mindful of the
ethical disclosure issues this may raise
• Any encounters with law enforcement
• Previous biomedical interventions around substance use (e.g. detoxification, OST, naltrexone, benzodiazepines, other medication for withdrawal)
• If history of OST is reported, enquire about: medication, frequency and dosage, duration of treatment and reflections of experience
• Previous psychosocial interventions (e.g. abstinence-based rehabilitation programmes, mutual or self-help groups)
2. Clinical consequences of • Accidents under the influence
use and relevant risk factor • Overdose
assessment • General – loss of weight
• Cardiovascular – deep venous thrombosis, hypertension, phlebitis, endocarditis, other cardiac complications. If considering methadone, ask
about: history of structural heart disease, arrhythmias, unexplained syncope, or medications/drugs that can prolong the QTc interval
• Respiratory – aspiration
• Gastro-intestinal – pancreatitis, recurrent gastritis, gastrointestinal bleeds
• Nervous system – peripheral neuropathy, any central nervous conditions
• Infectious – TB, HIV, hepatitis, and other blood-borne infections: testing history; diagnosis and treatment
• Consequences of injecting – vein damage, wounds, abscesses, overdose, etc.
3. Any mental-health-specific • Depression, anxiety and other common mental health conditions
diagnoses and interventions • Suicide
4. Withdrawal symptoms • Refer to Table 2-A3
5. Social circumstances and • Current living situation (homeless, shelter, with family, etc.)
support structures • Family, friend and clinical social support, both historic and current
• Current occupational/school/social structure (community, church, etc.) participation and social functioning.
OST, opioid substitution therapy; TB, tuberculosis; QTc, corrected QT interval.
†, If possible, and with consent, try to obtain collateral history, including from other clinicians.
TABLE 2-A3: Opioid withdrawal symptoms. 136
Early symptoms Late symptoms
Occurs within 6–12 hours for short-acting and within 30 hours for longer-acting opiates. Peaks within 72 h hours and usually lasts a week.
Symptoms include: Symptoms include:
• Tearing up and nose running • Nausea and vomiting
• Muscle aches • Diarrhoea
• Agitation and anxiety • Goosebumps
• Trouble falling and staying asleep • Stomach cramps
• Excessive yawning • Depression
• Sweats • Drug cravings
• Racing heart and hypertension
• Fever
TABLE 3-A3: Clinical assessment – differs, based on whether or not the patient is acutely ill. 81
Non-acute patients Acutely ill patients
Clinical assessment is routine, with attention to the following: Standard clinical assessment (alongside) is recommended, with attention to the reason for
• Any signs of hepatic, cardiac or neurological disease; any signs of presentation, in addition to that listed.
malnutrition • Clinical assessment:
• Needle site marks/scars or complications, including groin and neck ▪ Assess pupil reactions, basic signs (respiratory rate, heart rate, blood pressure, capillary refill).
• TB symptom screen and sputum sampling – because of the high burden ▪ Overdose: sleepiness, dilated pupils, sweating, hypotension
of TB in South Africa and likely under-diagnosis amongst people who ▪ Withdrawal reactions, including restlessness, sweating, excessive lacrimation, gooseflesh, dilated
use drugs, take sputum for Xpert MTB/RIF for diagnostic test pupils, muscle tenderness, increased heart rate and blood pressure
• Note: Opioid use may mask the symptoms of TB as opioids suppress the ▪ See the clinical opiate withdrawal scale: https://www.mdcalc.com/cows-score-opiate-
cough reflex; weight loss is common amongst people who use drugs; withdrawal#use-cases for an online tool
opioid withdrawal hot/cold flushes and fever may be like night sweats ▪ The OOWS has locally been found to have better inter-rater reliability: http://www.emcdda.
• HIV testing should be offered for those with unknown HIV status or europa.eu/attachements.cfm/att_35654_EN_OOWS.pdf
those with HIV-negative status who tested more than 6 weeks earlier • Laboratory assessment (all performed with relevant counselling and informed consent):
• Viral hepatitis testing: baseline HBsAg testing should be done, followed ▪ TB, HIV, HBV, HCV, syphilis; other infectious diseases as required
by vaccination for those who are not immune; HCV testing should be ▪ Monitoring tests in infected patients as per national guidelines
offered to all people with a history of injecting a substance or with ▪ In patients with risk factors for liver or renal disease (e.g. chronic alcohol use, chronic hepatitis
other risk factors† infection), concomitant medication with risk of hepatotoxicity/nephrotoxicity (e.g. TB and HIV
• Baseline ECG is recommended for patients with signs or symptoms treatment) or signs and symptoms of liver or renal disease (e.g. jaundice, pedal oedema, ascites):
suggestive of cardiac disease LFTs, with INR if evidence of dysfunction; FBC; creatinine
▪ Clinically directed testing as indicated
ECG, electrocardiogram; FBC, full blood count; HBsAg, hepatitis B surface antigen; HBV, hepatitis B virus; HCV, hepatitis C virus; INR, international normalised ratio; LFTs, liver function tests; MTB/
RIF Mycobacterium tuberculosis/rifampicin; TB, tuberculosis; OOWS, objective opioid withdrawal scale.
137
†, Individuals at higher risk for HCV, as per South African National Guidelines for the Management of Viral Hepatitis (2019) include: people who inject drugs; recipients of blood, blood products
and solid organ transplant before 1992; unsafe medical injection practices; occupational exposure; chronic haemodialysis; high-risk/traumatic sexual practices; men who have sex with men; use of
intranasal cocaine; piercing, tattooing or acupuncture; surgical procedures without proper sterilisation procedures, traditional/cultural practices such as circumcision and scarification rituals.
http://www.sajhivmed.org.za 113 Open Access