Page 122 - HIVMED_v21_i1.indb
P. 122
Page 31 of 34 Guideline
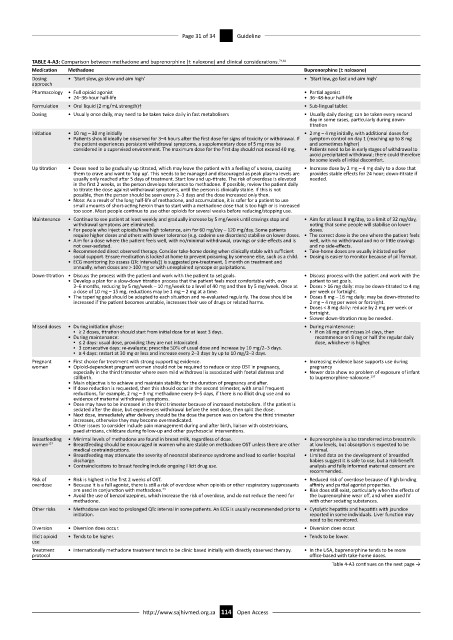
TABLE 4-A3: Comparison between methadone and buprenorphine (± naloxone) and clinical considerations. 74,81
Medication Methadone Buprenorphine (± naloxone)
Dosing • ‘Start slow, go slow and aim high’ • ‘Start low, go fast and aim high’
approach
Pharmacology • Full opioid agonist • Partial agonist
• 24–36-hour half-life • 36–48-hour half-life
Formulation • Oral liquid (2 mg/mL strength)† • Sub-lingual tablet
Dosing • Usually once daily, may need to be taken twice daily in fast metabolisers • Usually daily dosing; can be taken every second
day in some cases, particularly during down-
titration
Initiation • 10 mg – 30 mg initially • 2 mg – 4 mg initially, with additional doses for
• Patients should ideally be observed for 3–4 hours after the first dose for signs of toxicity or withdrawal. If symptom control on day 1 (reaching up to 8 mg
the patient experiences persistent withdrawal symptoms, a supplementary dose of 5 mg may be and sometimes higher)
considered in a supervised environment. The maximum dose for the first day should not exceed 40 mg. • Patients need to be in early stages of withdrawal to
avoid precipitated withdrawal; there could therefore
be some levels of initial discomfort.
Up titration • Doses need to be gradually up titrated, which may leave the patient with a feeling of unease, causing • Increase dose by 2 mg – 4 mg daily to a dose that
them to crave and want to ‘top up’. This needs to be managed and discouraged as peak plasma levels are provides stable effects for 24 hour; down-titrate if
usually only reached after 5 days of treatment. Start low and up-titrate. The risk of overdose is elevated needed.
in the first 2 weeks, as the person develops tolerance to methadone. If possible, review the patient daily
to titrate the dose against withdrawal symptoms, until the person is clinically stable. If this is not
possible, then the person should be seen every 2–3 days and the dose increased only then.
• Note: As a result of the long half-life of methadone, and accumulation, it is safer for a patient to use
small amounts of short-acting heroin than to start with a methadone dose that is too high or is increased
too soon. Most people continue to use other opioids for several weeks before reducing/stopping use.
Maintenance • Continue to see patient at least weekly and gradually increase by 5 mg/week until cravings stop and • Aim for at least 8 mg/day, to a limit of 32 mg/day,
withdrawal symptoms are eliminated. noting that some people will stabilise on lower
• For people who inject opioids/have high tolerance, aim for 60 mg/day – 120 mg/day. Some patients doses.
require higher doses and others with lower tolerance (e.g. codeine use disorders) stabilise on lower doses. • The correct dose is the one where the patient feels
• Aim for a dose where the patient feels well, with no/minimal withdrawal, cravings or side-effects and is well, with no withdrawal and no or little cravings
not over-sedated. and no side-effects.
• Recommended direct observed therapy. Consider take-home dosing when clinically stable with sufficient • Take-home doses are usually initiated earlier
social support. Ensure medication is locked at home to prevent poisoning by someone else, such as a child. • Dosing is easier to monitor because of pill format.
• ECG monitoring (to assess QTc intervals‡) is suggested pre-treatment, 1 month on treatment and
annually, when doses are > 100 mg or with unexplained syncope or palpitations.
Down-titration • Discuss the process with the patient and work with the patient to set goals. • Discuss process with the patient and work with the
• Develop a plan for a slow-down titration process that the patient feels most comfortable with, over patient to set goals.
3–6 months, reducing by 5 mg/week – 10 mg/week to a level of 40 mg and then by 5 mg/week. Once at • Doses > 16 mg daily: may be down-titrated to 4 mg
a dose of 10 mg – 15 mg, reductions may be 1 mg – 2 mg at a time. per week or fortnight.
• The tapering goal should be adapted to each situation and re-evaluated regularly. The dose should be • Doses 8 mg – 16 mg daily: may be down-titrated to
increased if the patient becomes unstable, increases their use of drugs or related harms. 2 mg – 4 mg per week or fortnight.
• Doses < 8 mg daily: reduce by 2 mg per week or
fortnight.
• Slower down-titration may be needed.
Missed doses • During initiation phase: • During maintenance:
▪ ≥ 2 doses, titration should start from initial dose for at least 3 days. ▪ If on ≥8 mg and misses ≥4 days, then
• During maintenance: recommence on 8 mg or half the regular daily
▪ ≤ 2 days: usual dose, providing they are not intoxicated. dose, whichever is higher.
▪ 3 consecutive days: re-evaluate; prescribe 50% of usual dose and increase by 10 mg/2–3 days.
▪ ≥ 4 days: restart at 30 mg or less and increase every 2–3 days by up to 10 mg/2–3 days.
Pregnant • First choice for treatment with strong supporting evidence. • Increasing evidence base supports use during
women • Opioid-dependent pregnant women should not be required to reduce or stop OST in pregnancy, pregnancy
especially in the third trimester where even mild withdrawal is associated with foetal distress and • Newer data show no problem of exposure of infant
stillbirth. to buprenorphine-naloxone. 137
• Main objective is to achieve and maintain stability for the duration of pregnancy and after.
• If dose reduction is requested, then this should occur in the second trimester, with small frequent
reductions, for example, 2 mg – 3 mg methadone every 3–5 days, if there is no illicit drug use and no
evidence of maternal withdrawal symptoms.
• Dose may have to be increased in the third trimester because of increased metabolism. If the patient is
sedated after the dose, but experiences withdrawal before the next dose, then split the dose.
• Next dose, immediately after delivery should be the dose the person was on before the third trimester
increases, otherwise they may become overmedicated.
• Other issues to consider include pain management during and after birth, liaison with obstetricians,
paediatricians, childcare during follow-up and other psychosocial interventions.
Breastfeeding • Minimal levels of methadone are found in breast milk, regardless of dose. • Buprenorphine is also transferred into breastmilk
women 137 • Breastfeeding should be encouraged in women who are stable on methadone OST unless there are other at low levels, but absorption is expected to be
medical contraindications. minimal.
• Breastfeeding may attenuate the severity of neonatal abstinence syndrome and lead to earlier hospital • Limited data on the development of breastfed
discharge. babies suggest it is safe to use, but a risk-benefit
• Contraindications to breast feeding include ongoing illicit drug use. analysis and fully informed maternal consent are
recommended.
Risk of • Risk is highest in the first 2 weeks of OST. • Reduced risk of overdose because of high binding
overdose • Because it is a full agonist, there is still a risk of overdose when opioids or other respiratory suppressants affinity and partial agonist properties.
are used in conjunction with methadone. 74 • Risk does still exist, particularly when the effects of
• Avoid the use of benzodiazepines, which increase the risk of overdose, and do not reduce the need for the buprenorphine wear off, and when used IV
methadone. with other sedating substances.
Other risks • Methadone can lead to prolonged QTc interval in some patients. An ECG is usually recommended prior to • Cytolytic hepatitis and hepatitis with jaundice
initiation. reported in some individuals. Liver function may
need to be monitored.
Diversion • Diversion does occur. • Diversion does occur.
Illicit opioid • Tends to be higher. • Tends to be lower.
use
Treatment • Internationally methadone treatment tends to be clinic based initially with directly observed therapy. • In the USA, buprenorphine tends to be more
protocol office-based with take-home doses.
Table 4-A3 continues on the next page →
http://www.sajhivmed.org.za 114 Open Access