Page 367 - HIVMED_v21_i1.indb
P. 367
Page 5 of 8 Original Research
TABLE 2: Univariate and multivariate analysis of patient characteristics associated
50 with high-risk human papillomavirus positivity.
43 Characteristic OR (95% CI) p** aOR (95% CI) p**
Number of Pa ents 30 13 15 17 Age bands (years) 3.0 (1.2–7.9) 0.02 2.9 (1.0–8.8) 0.05
40
22–29
-
-
30–45
-
-
20
0.17
46–60
1.6 (0.8–3.2)
0.50
1.2 (0.7–2.1)
10
Marital status
0 5 > 60 0.3 (0.1–1.5) 0.15 0.3 (0.1–1.7) 0.18
HPV HPV HPV HPV HPV Married 0.8 (0.5–1.3) 0.38 0.8 (0.4–1.5) 0.49
16 18/45 31/33/35/52/58 51/59 39/56/66/68 Single - - - -
Subtype grouping by channel Contraception
Non-hormonal - - - -
HPV, human papillomavirus. Hormonal 1.6 (0.9–2.7) 0.10 1.3 (0.7–2.6) 0.42
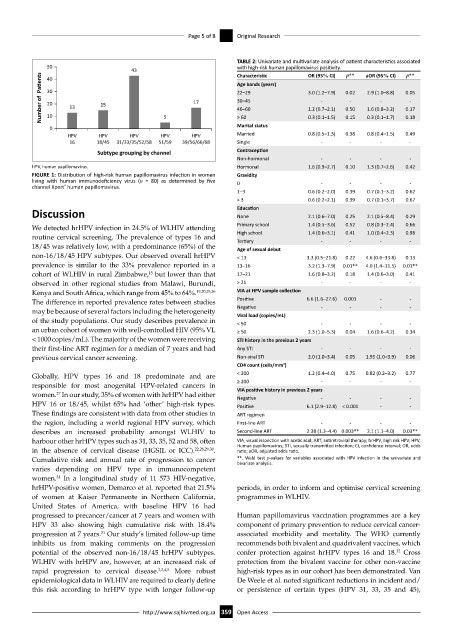
FIGURE 1: Distribution of high-risk human papillomavirus infection in women Gravidity
living with human immunodeficiency virus (n = 80) as determined by five 0 - - - -
channel Xpert human papillomavirus.
®
1–3 0.6 (0.2–2.0) 0.39 0.7 (0.1–3.2) 0.62
> 3 0.6 (0.2–2.1) 0.39 0.7 (0.1–3.7) 0.67
Discussion Education 2.1 (0.6–7.0) 0.25 2.1 (0.5–8.4) 0.29
None
Primary school 1.4 (0.5–3.6) 0.52 0.8 (0.3–2.4) 0.66
We detected hrHPV infection in 24.5% of WLHIV attending
routine cervical screening. The prevalence of types 16 and High school 1.4 (0.6–3.1) 0.41 1.0 (0.4–2.3) 0.98
-
-
-
Tertiary
-
18/45 was relatively low, with a predominance (65%) of the Age of sexual debut
non-16/18/45 HPV subtypes. Our observed overall hrHPV < 13 3.3 (0.5–21.8) 0.22 4.6 (0.6–33.8) 0.13
prevalence is similar to the 33% prevalence reported in a 13–16 3.2 (1.3–7.9) 0.01** 4.0 (1.4–11.5) 0.01**
15
cohort of WLHIV in rural Zimbabwe, but lower than that 17–21 1.6 (0.8–3.2) 0.18 1.4 (0.6–3.0) 0.41
observed in other regional studies from Malawi, Burundi, > 21 - - - -
Kenya and South Africa, which range from 45% to 64%. 19,20,25,26 VIA at HPV sample collection
The difference in reported prevalence rates between studies Positive 6.6 (1.6–27.6) 0.001 - -
may be because of several factors including the heterogeneity Negative - - - -
Viral load (copies/mL)
of the study populations. Our study describes prevalence in < 50 - - - -
an urban cohort of women with well-controlled HIV (95% VL ≥ 50 2.3 (1.0–5.3) 0.04 1.6 (0.6–4.2) 0.34
< 1000 copies/mL). The majority of the women were receiving STI history in the previous 2 years
their first-line ART regimen for a median of 7 years and had Any STI - - - -
previous cervical cancer screening. Non-viral STI 2.0 (1.0–3.4) 0.05 1.95 (1.0–3.9) 0.06
3
CD4 count (cells/mm )
Globally, HPV types 16 and 18 predominate and are < 200 1.2 (0.4–4.0) 0.75 0.82 (0.2–3.2) 0.77
responsible for most anogenital HPV-related cancers in ≥ 200 - - - -
VIA positive history in previous 2 years
27
women. In our study, 35% of women with hrHPV had either Negative - - - -
HPV 16 or 18/45, whilst 65% had ‘other’ high-risk types. Positive 6.1 (2.9–12.8) < 0.001 - -
These findings are consistent with data from other studies in ART regimen
the region, including a world regional HPV survey, which First-line ART - - - -
describes an increased probability amongst WLHIV to Second-line ART 2.38 (1.3–4.4) 0.003** 2.1 (1.1–4.0) 0.03**
harbour other hrHPV types such as 31, 33, 35, 52 and 58, often VIA, visual inspection with acetic acid; ART, antiretroviral therapy; hrHPV, high risk HPV; HPV,
Human papillomavirus; STI, sexually transmitted infection; CI, confidence interval; OR, odds
in the absence of cervical disease (HGSIL or ICC). 22,28,29,30 . ratio; aOR, adjusted odds ratio.
Cumulative risk and annual rate of progression to cancer **, Wald test p-values for variables associated with HPV infection in the univariate and
bivariate analysis.
varies depending on HPV type in immunocompetent
women. In a longitudinal study of 11 573 HIV-negative,
31
hrHPV-positive women, Demarco et al. reported that 21.5% periods, in order to inform and optimise cervical screening
of women at Kaiser Permanente in Northern California, programmes in WLHIV.
United States of America, with baseline HPV 16 had
progressed to precancer/cancer at 7 years and women with Human papillomavirus vaccination programmes are a key
HPV 33 also showing high cumulative risk with 18.4% component of primary prevention to reduce cervical cancer-
31
progression at 7 years. Our study’s limited follow-up time associated morbidity and mortality. The WHO currently
inhibits us from making comments on the progression recommends both bivalent and quadrivalent vaccines, which
32
potential of the observed non-16/18/45 hrHPV subtypes. confer protection against hrHPV types 16 and 18. Cross
WLHIV with hrHPV are, however, at an increased risk of protection from the bivalent vaccine for other non-vaccine
rapid progression to cervical disease. 2,3,4,5 More robust high-risk types as in our cohort has been demonstrated. Van
epidemiological data in WLHIV are required to clearly define De Weele et al. noted significant reductions in incident and/
this risk according to hrHPV type with longer follow-up or persistence of certain types (HPV 31, 33, 35 and 45),
http://www.sajhivmed.org.za 359 Open Access