Page 235 - SAHCS HIVMed Journal Vol 20 No 1 2019
P. 235
Page 4 of 6 Original Research
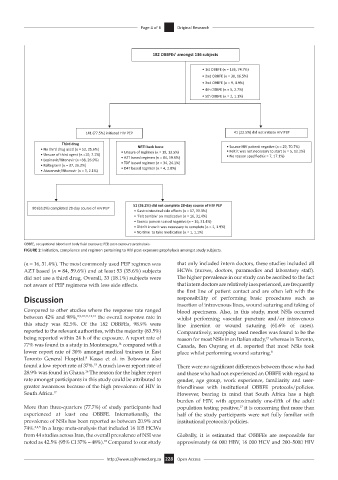
182 OBBFEs’ amongst 136 subjects
• 1st OBBFE (n = 136, 74.7%)
• 2nd OBBFE (n = 30, 16.5%)
• 3nd OBBFE (n = 9, 4.9%)
• 4th OBBFE (n = 5, 2.7%)
• 5th OBBFE (n = 2, 1.1%)
141 (77.5%) initiated HIV PEP 41 (22.5%) did not initiate HIV PEP
Third drug • Source HIV pa ent nega ve (n = 29, 70.7%)
• No third drug used (n = 53, 35.6%) NRTI back bone • Felt it was not necessary to start (n = 5, 12.2%)
• Unsure of third agent (n =10, 7.1%) • Unsure of regimen (n = 19, 13.5%) • No reason specified (n = 7, 17.1%)
• AZT based regimen (n = 84, 59.6%)
• Lopinavir/Ritonavir (n =38, 26.9%)
• Raltegravir (n = 37, 26.2%) • TDF based regimen (n = 34, 24.1%)
• Atazanavir/Ritonavir (n = 3, 2.1%) • D4T based regimen (n = 4, 2.8%)
51 (36.2%) did not complete 28-day course of HIV PEP
90 (63.8%) completed 28-day course of HIV PEP
• Gastrointes nal side effects (n = 17, 33.3%)
• ‘Felt terrible’ on medica on (n = 16, 31.4%)
• Source pa ent tested nega ve (n = 16, 31.4%)
• Didn’t know it was necessary to complete (n = 1, 1.9%)
• No me to take medica on (n = 1, 1.1%)
OBBFE, occupational blood and body fluid exposure; PEP, post-exposure prophylaxis.
FIGURE 1: Initiation, compliance and regimen pertaining to HIV post-exposure prophylaxis amongst study subjects.
(n = 16, 31.4%). The most commonly used PEP regimen was that only included intern doctors, these studies included all
AZT based (n = 84, 59.6%) and at least 53 (35.6%) subjects HCWs (nurses, doctors, paramedics and laboratory staff).
did not use a third drug. Overall, 33 (18.1%) subjects were The higher prevalence in our study can be ascribed to the fact
not aware of PEP regimens with less side effects. that intern doctors are relatively inexperienced, are frequently
the first line of patient contact and are often left with the
Discussion responsibility of performing basic procedures such as
insertion of intravenous lines, wound suturing and taking of
Compared to other studies where the response rate ranged blood specimens. Also, in this study, most NSIs occurred
between 42% and 98%, 8,9,10,11,12,13 the overall response rate in whilst performing vascular puncture and/or intravenous
this study was 82.5%. Of the 182 OBBFEs, 98.9% were line insertion or wound suturing (61.6% of cases).
reported to the relevant authorities, with the majority (83.5%) Comparatively, recapping used needles was found to be the
being reported within 24 h of the exposure. A report rate of reason for most NSIs in an Italian study, whereas in Toronto,
19
77% was found in a study in Montenegro, compared with a Canada, Ben Ouyang et al. reported that most NSIs took
14
lower report rate of 30% amongst medical trainees in East place whilst performing wound suturing. 8
Toronto General Hospital. Kassa et al. in Botswana also
8
found a low report rate of 37%. A much lower report rate of There were no significant differences between those who had
15
28.9% was found in Ghana. The reason for the higher report and those who had not experienced an OBBFE with regard to
16
rate amongst participants in this study could be attributed to gender, age group, work experience, familiarity and user-
greater awareness because of the high prevalence of HIV in friendliness with institutional OBBFE protocols/policies.
South Africa. 17 However, bearing in mind that South Africa has a high
burden of HIV, with approximately one-fifth of the adult
More than three-quarters (77.7%) of study participants had population testing positive, it is concerning that more than
17
experienced at least one OBBFE. Internationally, the half of the study participants were not fully familiar with
prevalence of NSIs has been reported as between 20.9% and institutional protocols/policies.
74%. 3,4,5 In a large meta-analysis that included 16 105 HCWs
from 44 studies across Iran, the overall prevalence of NSI was Globally, it is estimated that OBBFEs are responsible for
18
noted as 42.5% (95% CI 37% – 48%). Compared to our study approximately 66 000 HBV, 16 000 HCV and 200–5000 HIV
http://www.sajhivmed.org.za 228 Open Access