Page 378 - HIVMED_v21_i1.indb
P. 378
Page 3 of 9 Original Research
TABLE 1: Comparison of standard care and Teen Club care.
Standard care Teen Club
• Adolescents should have full disclosure by the age of 10–12 years; disclosure can • Adolescents should have full disclosure; this is a prerequisite for enrolment into the
be delayed depending on the cognitive ability of the adolescent Teen Club
• Goal-related transition from paediatric/adolescent to adult HIV services • Goal-related transition from paediatric/adolescent to adult HIV services
• Routine viral load monitoring and targeted viral load monitoring for suspected • Routine viral load monitoring and targeted viral load monitoring for suspected
treatment failure treatment failure
• Age-appropriate and developmentally appropriate adherence counselling • Age-appropriate and developmentally appropriate adherence counselling
• Lost to follow-up/defaulter tracking and tracing • Lost to follow-up/defaulter tracking and tracing
• HIV treatment literacy training of guardians and caregivers on treatment • HIV treatment literacy training of guardians and caregivers on treatment adherence,
adherence, disclosure and stigma issues disclosure and stigma issues
• Routine discussion with the children on their experience at school and future plans • Routine discussion with the child on their experience at school and future plans
• Linkage to relevant stakeholders and social support mechanisms in the community • Linkage to relevant stakeholders and social support mechanisms in the community
• Age-appropriate psychosocial support includes individualised and group • In addition to age-appropriate psychosocial support offered in standard care, the Teen
counselling on issues such as treatment failure counselling, opportunistic Club:
infections, STIs, SRH, alcohol use and abuse, mental health, child protection
and other topics according to the adolescents’ needs. ▪ Meets once a month on a Friday or Saturday in ‘safe spaces’ at the clinic
▪ Shares challenges, fears, experiences and coping mechanisms during monthly
meetings
▪ Has special talks or presentation of ALHIV-related topics from subject matter experts
▪ Has access to information, education and communication materials, such as videos
and dramas/acts on adolescence and HIV, followed by discussions
▪ Occasionally participates in Teen Club retreats and trips where recreational activities
and life stories are shared
ALHIV, adolescents living with HIV; SRH, sexual and reproductive health; STIs, sexually transmitted infections.
Guidelines, the HIV disclosure process of the child must be a
carefully planned process that informs the child of their HIV Electronic pa ent monitoring system (ePMS) with all clients on ART
status and why they have to take their HIV medication. The at intermediate hospital katutura paediatric ART clinic (N ≈ 720)
process must take into account the individual’s maturity,
understanding of HIV and their social support system, and Selected all adolescents (10–19 years) who were on ART at
19
should be initiated as early as 6–10 years of age. Once the clinic between 1 July 2015 and 30 June 2017 (N = 482)
adolescents are aware that they are HIV infected, they can
enrol in the Teen Club. Ninety-seven excluded
adolescents who were
transferred in from other
Participants’ selection facili es to the clinic
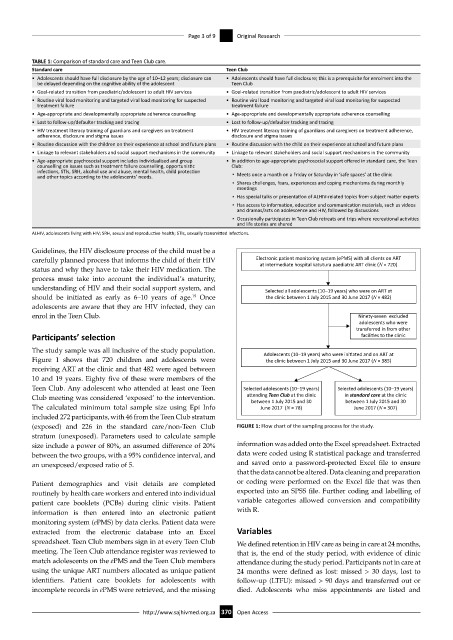
The study sample was all inclusive of the study population. Adolescents (10–19 years) who were ini ated and on ART at
Figure 1 shows that 720 children and adolescents were the clinic between 1 July 2015 and 30 June 2017 (N = 385)
receiving ART at the clinic and that 482 were aged between
10 and 19 years. Eighty five of these were members of the
Teen Club. Any adolescent who attended at least one Teen Selected adolescents (10–19 years) Selected adolescents (10–19 years)
Club meeting was considered ‘exposed’ to the intervention. aending Teen Club at the clinic in standard care at the clinic
between 1 July 2015 and 30
between 1 July 2015 and 30
The calculated minimum total sample size using Epi Info June 2017 (N = 78) June 2017 (N = 307)
included 272 participants, with 46 from the Teen Club stratum
(exposed) and 226 in the standard care/non-Teen Club FIGURE 1: Flow chart of the sampling process for the study.
stratum (unexposed). Parameters used to calculate sample
size include a power of 80%, an assumed difference of 20% information was added onto the Excel spreadsheet. Extracted
between the two groups, with a 95% confidence interval, and data were coded using R statistical package and transferred
an unexposed/exposed ratio of 5. and saved onto a password-protected Excel file to ensure
that the data cannot be altered. Data cleaning and preparation
Patient demographics and visit details are completed or coding were performed on the Excel file that was then
routinely by health care workers and entered into individual exported into an SPSS file. Further coding and labelling of
patient care booklets (PCBs) during clinic visits. Patient variable categories allowed conversion and compatibility
information is then entered into an electronic patient with R.
monitoring system (ePMS) by data clerks. Patient data were
extracted from the electronic database into an Excel Variables
spreadsheet. Teen Club members sign in at every Teen Club We defined retention in HIV care as being in care at 24 months,
meeting. The Teen Club attendance register was reviewed to that is, the end of the study period, with evidence of clinic
match adolescents on the ePMS and the Teen Club members attendance during the study period. Participants not in care at
using the unique ART numbers allocated as unique patient 24 months were defined as lost: missed > 30 days, lost to
identifiers. Patient care booklets for adolescents with follow-up (LTFU): missed > 90 days and transferred out or
incomplete records in ePMS were retrieved, and the missing died. Adolescents who miss appointments are listed and
http://www.sajhivmed.org.za 370 Open Access