Page 344 - HIVMED_v21_i1.indb
P. 344
Page 3 of 5 Original Research
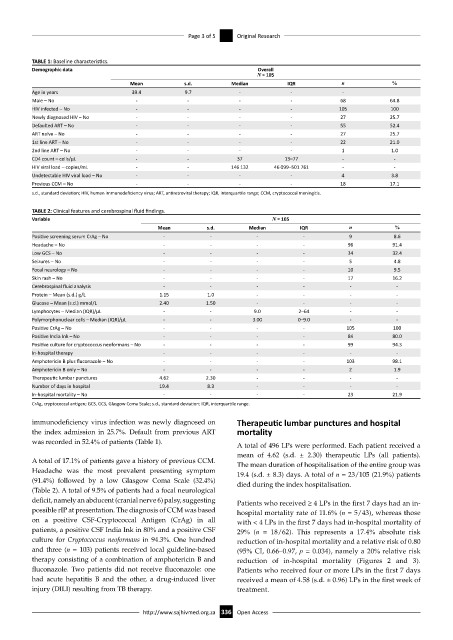
TABLE 1: Baseline characteristics.
Demographic data Overall
N = 105
Mean s.d. Median IQR n %
Age in years 39.4 9.7 - - -
Male – No - - - - 68 64.8
HIV infected – No - - - - 105 100
Newly diagnosed HIV – No - - - - 27 25.7
Defaulted ART – No - - - - 55 52.4
ART naïve – No - - - - 27 25.7
1st line ART – No - - - - 22 21.0
2nd line ART – No - - - - 1 1.0
CD4 count – cells/µL - - 37 13–77 - -
HIV viral load – copies/mL - - 146 132 46 099–501 761 - -
Undetectable HIV viral load – No - - - - 4 3.8
Previous CCM – No - - - - 18 17.1
s.d., standard deviation; HIV, human immunodeficiency virus; ART, antiretroviral therapy; IQR, interquartile range; CCM, cryptococcal meningitis.
TABLE 2: Clinical features and cerebrospinal fluid findings.
Variable N = 105
Mean s.d. Median IQR n %
Positive screening serum CrAg – No - - - - 9 8.6
Headache – No - - - - 96 91.4
Low GCS – No - - - - 34 32.4
Seizures – No - - - - 5 4.8
Focal neurology – No - - - - 10 9.5
Skin rash – No - - - - 17 16.2
Cerebrospinal fluid analysis - - - - - -
Protein – Mean (s.d.) g/L 1.15 1.0 - - - -
Glucose – Mean (s.d.) mmol/L 2.40 1.50 - - - -
Lymphocytes – Median (IQR)/µL - - 9.0 2–64 - -
Polymorphonuclear cells – Median (IQR)/µL - - 3.00 0–9.0 - -
Positive CrAg – No - - - - 105 100
Positive India Ink – No - - - - 84 80.0
Positive culture for cryptococcus neoformans – No - - - - 99 94.3
In-hospital therapy - - - - - -
Amphotericin B plus fluconazole – No - - - - 103 98.1
Amphotericin B only – No - - - - 2 1.9
Therapeutic lumbar punctures 4.62 2.30 - - - -
Number of days in hospital 19.4 8.3 - - - -
In-hospital mortality – No - - - - 23 21.9
CrAg, cryptococcal antigen; GCS, GCS, Glasgow Coma Scale; s.d., standard deviation; IQR, interquartile range.
immunodeficiency virus infection was newly diagnosed on Therapeutic lumbar punctures and hospital
the index admission in 25.7%. Default from previous ART mortality
was recorded in 52.4% of patients (Table 1).
A total of 496 LPs were performed. Each patient received a
mean of 4.62 (s.d. ± 2.30) therapeutic LPs (all patients).
A total of 17.1% of patients gave a history of previous CCM. The mean duration of hospitalisation of the entire group was
Headache was the most prevalent presenting symptom 19.4 (s.d. ± 8.3) days. A total of n = 23/105 (21.9%) patients
(91.4%) followed by a low Glasgow Coma Scale (32.4%) died during the index hospitalisation.
(Table 2). A total of 9.5% of patients had a focal neurological
deficit, namely an abducent (cranial nerve 6) palsy, suggesting Patients who received ≥ 4 LPs in the first 7 days had an in-
possible rIP at presentation. The diagnosis of CCM was based hospital mortality rate of 11.6% (n = 5/43), whereas those
on a positive CSF-Cryptococcal Antigen (CrAg) in all with < 4 LPs in the first 7 days had in-hospital mortality of
patients, a positive CSF India Ink in 80% and a positive CSF 29% (n = 18/62). This represents a 17.4% absolute risk
culture for Cryptococcus neoformans in 94.3%. One hundred reduction of in-hospital mortality and a relative risk of 0.80
and three (n = 103) patients received local guideline-based (95% CI, 0.66–0.97, p = 0.034), namely a 20% relative risk
therapy consisting of a combination of amphotericin B and reduction of in-hospital mortality (Figures 2 and 3).
fluconazole. Two patients did not receive fluconazole: one Patients who received four or more LPs in the first 7 days
had acute hepatitis B and the other, a drug-induced liver received a mean of 4.58 (s.d. ± 0.96) LPs in the first week of
injury (DILI) resulting from TB therapy. treatment.
http://www.sajhivmed.org.za 336 Open Access