Page 296 - HIVMED_v21_i1.indb
P. 296
Page 6 of 10 Original Research
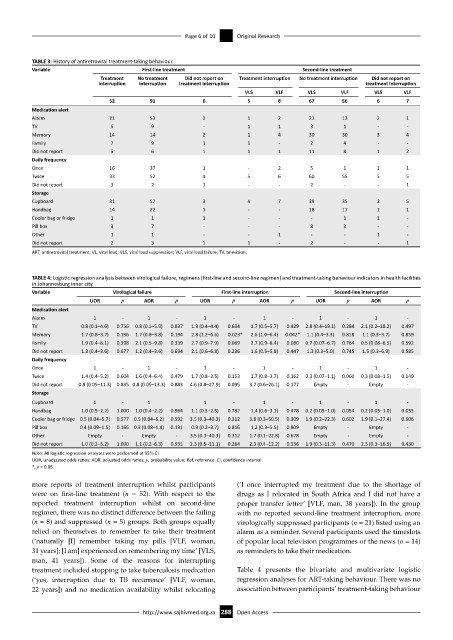
TABLE 3: History of antiretroviral treatment-taking behaviour.
Variable First-line treatment Second-line treatment
Treatment No treatment Did not report on Treatment interruption No treatment interruption Did not report on
interruption interruption treatment interruption treatment interruption
VLS VLF VLS VLF VLS VLF
52 91 6 5 8 67 56 6 7
Medication alert
Alarm 21 53 2 1 2 21 13 2 1
TV 5 9 - 1 1 3 1 - -
Memory 14 14 2 1 4 30 30 3 4
Family 7 9 1 1 - 2 4 - -
Did not report 5 6 1 1 1 11 8 1 2
Daily frequency
Once 16 37 1 - 2 5 1 1 1
Twice 33 52 4 5 6 60 55 5 5
Did not report 3 2 1 - - 2 - - 1
Storage
Cupboard 31 57 3 4 7 39 35 3 5
Handbag 14 22 1 - - 18 17 1 1
Cooler bag or fridge 1 1 1 - - - 1 1 -
Pill box 3 7 - - - 8 3 - -
Other 1 1 - - 1 - - 1 -
Did not report 2 3 1 1 - 2 - - 1
ART, antiretroviral treatment; VL, viral load; VLS, viral load suppression; VLF, viral load failure; TV, television.
TABLE 4: Logistic regression analysis between virological failure, regimens (first-line and second-line regimen) and treatment-taking behaviour indicators in health facilities
in Johannesburg inner city.
Variable Virological failure First-line interruption Second-line interruption
UOR p AOR p UOR p AOR p UOR p AOR p
Medication alert
Alarm 1 - 1 - 1 - 1 - 1 - 1 -
TV 0.8 (0.1–4.6) 0.756 0.8 (0.1–5.5) 0.837 1.3 (0.4–4.4) 0.634 1.7 (0.5–5.7) 0.429 2.8 (0.4–19.1) 0.284 2.1 (0.2–18.2) 0.497
Memory 1.7 (0.8–3.7) 0.196 1.7 (0.8–3.8) 0.194 2.8 (1.2–6.6) 0.023* 2.6 (1.0–6.4) 0.042* 1.1 (0.4–3.3) 0.818 1.1 (0.3–3.7) 0.859
Family 1.9 (0.4–8.1) 0.398 2.1 (0.5–9.8) 0.339 2.7 (0.9–7.9) 0.069 2.7 (0.9–8.4) 0.080 0.7 (0.07–6.7) 0.764 0.5 (0.08–6.5) 0.592
Did not report 1.3 (0.4–3.6) 0.677 1.2 (0.4–3.6) 0.694 2.1 (0.6–6.8) 0.236 1.6 (0.5–5.8) 0.447 1.3 (0.3–5.0) 0.745 1.5 (0.3–6.9) 0.585
Daily frequency
Once 1 - 1 - 1 - 1 - 1 - 1 -
Twice 1.4 (0.4–5.2) 0.604 1.6 (0.4–6.4) 0.479 1.7 (0.8–3.5) 0.153 1.7 (0.8–3.7) 0.162 0.3 (0.07–1.1) 0.060 0.3 (0.08–1.5) 0.149
Did not report 0.8 (0.05–11.3) 0.835 0.8 (0.05–13.3) 0.883 4.6 (0.8–27.9) 0.095 3.7 (0.6–26.1) 0.177 Empty - Empty -
Storage
Cupboard 1 - 1 1 - 1 - 1 - 1 -
Handbag 1.0 (0.5–2.2) 1.000 1.0 (0.4–2.2) 0.964 1.1 (0.5–2.5) 0.782 1.4 (0.6–3.1) 0.478 0.2 (0.05–1.0) 0.054 0.2 (0.05–1.0) 0.055
Cooler bag or fridge 0.5 (0.04–5.7) 0.577 0.5 (0.04–6.2) 0.592 3.5 (0.3–40.3) 0.312 3.8 (0.3–50.5) 0.309 1.9 (0.2–22.3) 0.602 1.9 (0.1–27.4) 0.606
Pill box 0.4 (0.09–1.5) 0.166 0.3 (0.08–1.4) 0.131 0.9 (0.2–3.7) 0.816 1.2 (0.3–5.5) 0.809 Empty - Empty -
Other Empty - Empty - 3.5 (0.3–40.3) 0.312 1.7 (0.1–22.8) 0.678 Empty - Empty -
Did not report 1.0 (0.2–5.2) 1.000 1.1 (0.2–6.3) 0.931 2.3 (0.5–11.1) 0.284 2.3 (0.4–12.2) 0.336 1.9 (0.3–11.3) 0.470 2.3 (0.3–16.9) 0.430
Note: All logistic regression analyses were performed at 95% CI.
UOR, unadjusted odds ratios; AOR, adjusted odds ratios; p, probability value; Ref, reference; CI, confidence interval.
*, p < 0.05.
more reports of treatment interruption whilst participants (‘I once interrupted my treatment due to the shortage of
were on first-line treatment (n = 52). With respect to the drugs as I relocated in South Africa and I did not have a
reported treatment interruption whilst on second-line proper transfer letter’ [VLF, man, 38 years]). In the group
regimen, there was no distinct difference between the failing with no reported second-line treatment interruption, more
(n = 8) and suppressed (n = 5) groups. Both groups equally virologically suppressed participants (n = 21) listed using an
relied on themselves to remember to take their treatment alarm as a reminder. Several participants used the timeslots
(‘naturally [I] remember taking my pills [VLF, woman, of popular local television programmes or the news (n = 14)
31 years]; [I am] experienced on remembering my time’ [VLS, as reminders to take their medication.
man, 41 years]). Some of the reasons for interrupting
treatment included stopping to take tuberculosis medication Table 4 presents the bivariate and multivariate logistic
(‘yes, interruption due to TB recurrence’ [VLF, woman, regression analyses for ART-taking behaviour. There was no
22 years]) and no medication availability whilst relocating association between participants’ treatment-taking behaviour
http://www.sajhivmed.org.za 288 Open Access