Page 242 - HIVMED_v21_i1.indb
P. 242
Page 4 of 9 Review Article
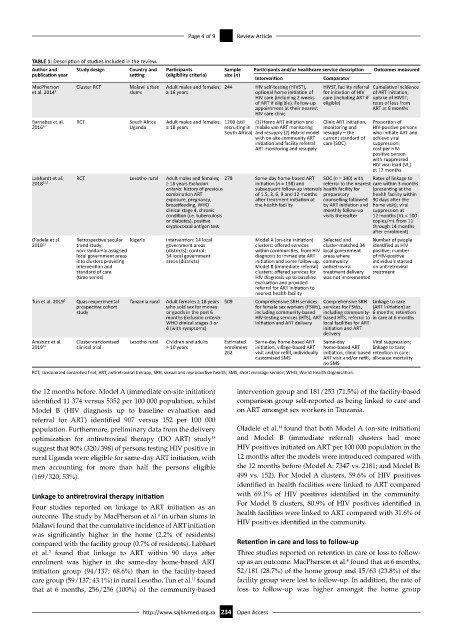
TABLE 1: Description of studies included in the review.
Author and Study design Country and Participants Sample Participants and/or healthcare service description Outcomes measured
publication year setting (eligibility criteria) size (n)
Intervention Comparator
MacPherson Cluster RCT Malawi urban Adult males and females; 244 HIV self-testing (HIVST), HIVST, facility referral Cumulative incidence
et al. 2014 4 slums ≥ 16 years optional home initiation of for initiation of HIV of ART initiation;
HIV care (including 2 weeks care (including ART if uptake of HIVST;
of ART if eligible). Follow-up eligible) rates of loss from
appointment at their nearest ART at 6 months
HIV care clinic
Barnabas et al. RCT South Africa Adult males and females; 1200 (still (1) Home ART initiation and Clinic ART initiation, Proportion of
2016 6,7 Uganda ≥ 18 years recruiting in mobile van ART monitoring monitoring and HIV-positive persons
South Africa) and resupply (2) Hybrid model resupply – the who initiate ART and
with on-site community ART current standard of achieve viral
initiation and facility referral care (SOC) suppression;
ART monitoring and resupply cost per HIV-
positive person
with suppressed
HIV viral load (VL)
at 12 months
Labhardt et al. RCT Lesotho rural Adult males and females; 278 Same-day home-based ART SOC (n = 140) with Rates of linkage to
2018 3,12 ≥ 18 years Exclusion initiation (n = 138) and referral to the nearest care within 3 months
criteria: history of previous subsequent follow-up intervals health facility for (presenting at the
combination ART of 1.5, 3, 6, 9 and 12 months preparatory health facility within
exposure, pregnancy, after treatment initiation at counselling followed 90 days after the
breastfeeding, WHO the health facility by ART initiation and home visit); viral
clinical stage 4, chronic monthly follow-up suppression at
condition (i.e. tuberculosis visits thereafter 12 months (VL < 100
or diabetes), positive copies/mL from 11
cryptococcal antigen test through 14 months
after enrolment)
Oladele et al. Retrospective secular Nigeria Intervention: 14 local Model A (on-site initiation) Selected and Number of people
2018 11 trend study; government areas clusters: offered services cluster-matched 34 identified as HIV
non-randomly assigned (districts); control: within communities, from HIV local government positive; number
local government areas 34 local government diagnosis to immediate ART areas where of HIV-positive
into clusters providing areas (districts) initiation and some follow-up. community individuals started
intervention and Model B (immediate referral) antiretroviral on antiretroviral
standard of care clusters: offered services for treatment delivery treatment
(time series) HIV diagnosis up to baseline was not implemented
evaluation and provided
referral for ART initiation to
nearest health facility
Tun et al. 2019 9 Quasi-experimental Tanzania rural Adult females ≥ 18 years 509 Comprehensive SRH services Comprehensive SRH Linkage to care
prospective cohort who sold sex for money for female sex workers (FSWs), services for FSWs, (ART initiation) at
study or goods in the past 6 including community-based including community- 6 months; retention
months Exclusion criteria: HIV-testing services (HTS), ART based HTS, referral to in care at 6 months
WHO clinical stages 3 or initiation and ART delivery local facilities for ART
4 (with symptoms) initiation and ART
delivery
Amstutz et al. Cluster-randomised Lesotho rural Children and adults Estimated Same-day home-based ART Same-day Viral suppression;
2019 10 clinical trial > 10 years enrolment: initiation, village-based ART home-based ART linkage to care;
262 visit and/or refill, individually initiation, clinic-based retention in care;
customised SMS ART visit and/or refill, all-cause mortality
no SMS
RCT, randomised controlled trial; ART, antiretroviral therapy; SRH, sexual and reproductive health; SMS, short message service; WHO, World Health Organisation.
the 12 months before. Model A (immediate on-site initiation) intervention group and 181/253 (71.5%) of the facility-based
identified 11 374 versus 5352 per 100 000 population, whilst comparison group self-reported as being linked to care and
Model B (HIV diagnosis up to baseline evaluation and on ART amongst sex workers in Tanzania.
referral for ART) identified 907 versus 152 per 100 000
14
population. Furthermore, preliminary data from the delivery Oladele et al. found that both Model A (on-site initiation)
optimization for antiretroviral therapy (DO ART) study and Model B (immediate referral) clusters had more
13
suggest that 80% (320/398) of persons testing HIV positive in HIV positives initiated on ART per 100 000 population in the
rural Uganda were eligible for same-day ART initiation, with 12 months after the models were introduced compared with
men accounting for more than half the persons eligible the 12 months before (Model A: 7347 vs. 2181; and Model B:
(169/320; 53%). 499 vs. 152). For Model A clusters, 59.6% of HIV positives
identified in health facilities were linked to ART compared
Linkage to antiretroviral therapy initiation with 69.1% of HIV positives identified in the community.
Four studies reported on linkage to ART initiation as an For Model B clusters, 80.9% of HIV positives identified in
outcome. The study by MacPherson et al. in urban slums in health facilities were linked to ART compared with 31.6% of
4
Malawi found that the cumulative incidence of ART initiation HIV positives identified in the community.
was significantly higher in the home (2.2% of residents)
compared with the facility group (0.7% of residents). Labhart Retention in care and loss to follow-up
et al. found that linkage to ART within 90 days after Three studies reported on retention in care or loss to follow-
3
4
enrolment was higher in the same-day home-based ART up as an outcome. MacPherson et al. found that at 6 months,
initiation group (94/137; 68.6%) than in the facility-based 52/181 (28.7%) of the home group and 15/63 (23.8%) of the
care group (59/137; 43.1%) in rural Lesotho. Tun et al. found facility group were lost to follow-up. In addition, the rate of
11
that at 6 months, 256/256 (100%) of the community-based loss to follow-up was higher amongst the home group
http://www.sajhivmed.org.za 234 Open Access