Page 26 - SAHCS HIVMed Journal Vol 20 No 1 2019
P. 26
Page 13 of 16 Guideline
Detailed recommendations opening pressures. Patients with persistent pressure
symptoms and measured high opening pressures who fail to
Measurement of opening pressure
respond to daily LPs for more than 1 week may require
The panel agreed that it is a good practice to measure the CSF lumbar drain insertion or shunting procedures. In such cases,
opening pressure whenever a diagnostic LP is performed. neurosurgical consultation should be sought.
However, in practice, the opening pressure may not have
been measured at the initial diagnostic LP. Thus, once the Recommendation 7: Management
diagnosis of CM is made, an LP should be repeated to
measure CSF opening pressure, particularly if the patient still of relapse episodes of cryptococcal
has a headache (which is usually the case). The pressure meningitis
should be measured using a manometer with the patient
lying down and without excessive spinal flexion. There are several possible reasons for recurrence of symptoms
Approximately 15% of patients with initially normal of meningitis among patients treated for CM. In certain cases,
intracranial pressure will develop raised intracranial pressure recurrence is caused by microbiological relapse (although
during treatment; thus, all patients should be monitored this is very uncommon with good adherence to maintenance
daily for headache or signs of raised intracranial pressure fluconazole). There are situations in which there is a
that should prompt an LP. recurrence of symptoms but CSF fungal cultures are negative.
The causes are summarised in Table 10.
What to do if a manometer is unavailable?
Manometers are not readily available in all centres or settings. Initial assessment
In the absence of a manometer, the CSF pressure can be When a patient seeks care for a recurrent episode of
crudely estimated in various ways: meningitis, it is not always possible to immediately be sure
what the aetiology is. The initial assessment should include:
• Drop counting: obtaining ≥ 40 drops of free-flowing CSF
in 60 s using a 22-gauge spinal needle suggests a high CSF • An evaluation of the patient’s adherence to fluconazole
pressure. 63 consolidation and maintenance phase treatment (using
• An ‘eyeball test’: a powerful squirt of CSF from the LP self-reported and pharmacy refill data).
needle suggests a high CSF pressure. • An enquiry as to whether the patient has recently started
• Makeshift manometers from intravenous line sets can be ART to support a possible IRIS diagnosis.
used to estimate opening pressure in cm H O although • An LP to measure opening pressure, assess CSF
2
these sets consistently under-estimate the opening inflammation and for a prolonged fungal culture (request
pressure. 64
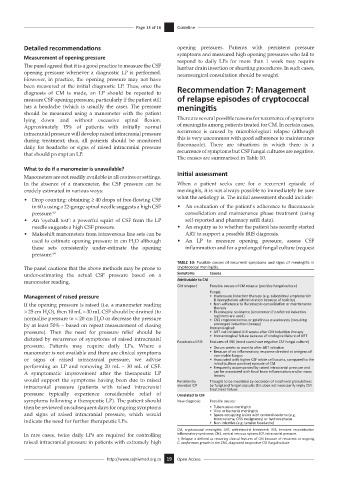
TABLE 10: Possible causes of recurrent symptoms and signs of meningitis in
The panel cautions that the above methods may be prone to cryptococcal meningitis.
under-estimating the actual CSF pressure based on a Symptoms Causes
manometer reading. Attributable to CM
CM relapse† Possible causes of CM relapse (positive fungal culture)
Fungal:
Management of raised pressure • Inadequate induction therapy (e.g. suboptimal amphotericin
B deoxycholate administration because of toxicity)
If the opening pressure is raised (i.e. a manometer reading • Non-adherence to fluconazole consolidation or maintenance
therapy
> 25 cm H O), then 10 mL – 30 mL CSF should be drained (to • Fluconazole resistance (uncommon if preferred induction
2
normalise pressure to < 20 cm H O or decrease the pressure regimens are used)
2 • CNS cryptococcomas or gelatinous pseudocysts (requiring
prolonged induction therapy)
by at least 50% – based on repeat measurement of closing Immunological:
pressure). Then the need for pressure relief should be • ART not initiated 4–6 weeks after CM induction therapy
dictated by recurrence of symptoms of raised intracranial Paradoxical IRIS • Immunological failure because of virological failure of ART
Features of IRIS (most cases have negative CSF fungal culture)
pressure. Patients may require daily LPs. Where a • Occurs weeks to months after ART initiation
manometer is not available and there are clinical symptoms • Because of an inflammatory response directed at antigens of
non-viable fungus
or signs of raised intracranial pressure, we advise • Associated with higher CSF white cell counts, compared to the
initial (culture positive) episode of CM
performing an LP and removing 20 mL – 30 mL of CSF. • Frequently accompanied by raised intracranial pressure and
A symptomatic improvement after the therapeutic LP can be associated with focal brain inflammation and/or mass
lesions
would support the symptoms having been due to raised Persistently Thought to be mediated by occlusion of arachnoid granulations
intracranial pressure (patients with raised intracranial elevated ICP by fungi and fungal capsule; this does not necessarily imply CM
treatment failure.
pressure typically experience considerable relief of Unrelated to CM
symptoms following a therapeutic LP). The patient should New diagnosis Possible causes:
then be reviewed on subsequent days for ongoing symptoms • Tuberculous meningitis
• Viral or bacterial meningitis
and signs of raised intracranial pressure, which would • Space-occupying lesion with cerebral oedema (e.g.
tuberculoma, CNS malignancy) or hydrocephalus
indicate the need for further therapeutic LPs. • Non-infective (e.g. tension headache)
CM, cryptococcal meningitis; ART, antiretroviral treatment; IRIS, immune reconstitution
In rare cases, twice daily LPs are required for controlling inflammatory syndrome; CNS, central nervous system; ICP, intracranial pressure.
raised intracranial pressure in patients with extremely high †, Relapse is defined as recurring clinical features of CM because of recurrent or ongoing
C. neoformans growth in the CNS, diagnosed on positive CSF fungal culture.
http://www.sajhivmed.org.za 19 Open Access