Page 76 - HIVMED_v21_i1.indb
P. 76
Page 3 of 8 Guideline
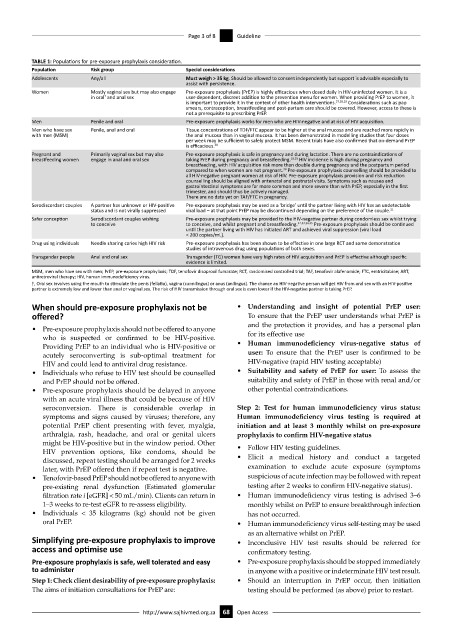
TABLE 1: Populations for pre-exposure prophylaxis consideration.
Population Risk group Special considerations
Adolescents Any/all Must weigh > 35 kg. Should be allowed to consent independently but support is advisable especially to
assist with persistence.
Women Mostly vaginal sex but may also engage Pre-exposure prophylaxis (PrEP) is highly efficacious when dosed daily in HIV-uninfected women. It is a
in oral and anal sex user-dependent, discreet addition to the prevention menu for women. When providing PrEP to women, it
†
is important to provide it in the context of other health interventions. 27,28,29 Considerations such as pap
smears, contraception, breastfeeding and post-partum care should be covered. However, access to these is
not a prerequisite to prescribing PrEP.
Men Penile and oral Pre-exposure prophylaxis works for men who are HIV-negative and at risk of HIV acquisition.
Men who have sex Penile, anal and oral Tissue concentrations of TDF/FTC appear to be higher at the anal mucosa and are reached more rapidly in
with men (MSM) the anal mucosa than in vaginal mucosa. It has been demonstrated in modelling studies that four doses
per week may be sufficient to safely protect MSM. Recent trials have also confirmed that on-demand PrEP
is efficacious. 28
Pregnant and Primarily vaginal sex but may also Pre-exposure prophylaxis is safe in pregnancy and during lactation. There are no contraindications of
breastfeeding women engage in anal and oral sex taking PrEP during pregnancy and breastfeeding. 19,25 HIV incidence is high during pregnancy and
breastfeeding, with HIV acquisition risk more than double during pregnancy and the postpartum period
compared to when women are not pregnant. Pre-exposure prophylaxis counselling should be provided to
30
all HIV-negative pregnant women at risk of HIV. Pre-exposure prophylaxis provision and risk reduction
counselling should be aligned with antenatal and postnatal visits. Symptoms such as nausea and
gastrointestinal symptoms are far more common and more severe than with PrEP, especially in the first
trimester, and should thus be actively managed.
There are no data yet on TAF/FTC in pregnancy.
Serodiscordant couples A partner has unknown or HIV-positive Pre-exposure prophylaxis may be used as a ‘bridge’ until the partner living with HIV has an undetectable
status and is not virally suppressed viral load – at that point PrEP may be discontinued depending on the preference of the couple. 31
Safer conception Serodiscordant couples wishing Pre-exposure prophylaxis may be provided to the HIV-negative partner during condomless sex whilst trying
to conceive to conceive, and whilst pregnant and breastfeeding. 32,33,34,35 Pre-exposure prophylaxis should be continued
until the partner living with HIV has initiated ART and achieved viral suppression (viral load
< 200 copies/mL).
Drug using individuals Needle sharing caries high HIV risk Pre-exposure prophylaxis has been shown to be effective in one large RCT and some demonstration
studies of intravenous drug using populations of both sexes.
Transgender people Anal and oral sex Transgender (TG) women have very high rates of HIV acquisition and PrEP is effective although specific
evidence is limited.
MSM, men who have sex with men; PrEP, pre-exposure prophylaxis; TDF, tenofovir disoproxil fumarate; RCT, randomised controlled trial; TAF, tenofovir alafenamide; FTC, emtricitabine; ART,
antiretroviral therapy; HIV, human immunodeficiency virus.
†, Oral sex involves using the mouth to stimulate the penis (fellatio), vagina (cunnilingus) or anus (anilingus). The chance an HIV-negative person will get HIV from oral sex with an HIV-positive
partner is extremely low and lower than anal or vaginal sex. The risk of HIV transmission through oral sex is even lower if the HIV-negative partner is taking PrEP.
When should pre-exposure prophylaxis not be • Understanding and insight of potential PrEP user:
offered? To ensure that the PrEP user understands what PrEP is
and the protection it provides, and has a personal plan
• Pre-exposure prophylaxis should not be offered to anyone
who is suspected or confirmed to be HIV-positive. for its effective use
Providing PrEP to an individual who is HIV-positive or • Human immunodeficiency virus-negative status of
acutely seroconverting is sub-optimal treatment for user: To ensure that the PrEP user is confirmed to be
HIV and could lead to antiviral drug resistance. HIV-negative (rapid HIV testing acceptable)
• Individuals who refuse to HIV test should be counselled • Suitability and safety of PrEP for user: To assess the
and PrEP should not be offered. suitability and safety of PrEP in those with renal and/or
• Pre-exposure prophylaxis should be delayed in anyone other potential contraindications.
with an acute viral illness that could be because of HIV
seroconversion. There is considerable overlap in Step 2: Test for human immunodeficiency virus status:
symptoms and signs caused by viruses; therefore, any Human immunodeficiency virus testing is required at
potential PrEP client presenting with fever, myalgia, initiation and at least 3 monthly whilst on pre-exposure
arthralgia, rash, headache, and oral or genital ulcers prophylaxis to confirm HIV-negative status
might be HIV-positive but in the window period. Other • Follow HIV testing guidelines.
HIV prevention options, like condoms, should be
discussed, repeat testing should be arranged for 2 weeks • Elicit a medical history and conduct a targeted
later, with PrEP offered then if repeat test is negative. examination to exclude acute exposure (symptoms
• Tenofovir-based PrEP should not be offered to anyone with suspicious of acute infection may be followed with repeat
pre-existing renal dysfunction (Estimated glomerular testing after 2 weeks to confirm HIV-negative status).
filtration rate i [eGFR] < 50 mL/min). Clients can return in • Human immunodeficiency virus testing is advised 3–6
1–3 weeks to re-test eGFR to re-assess eligibility. monthly whilst on PrEP to ensure breakthrough infection
• Individuals < 35 kilograms (kg) should not be given has not occurred.
oral PrEP. • Human immunodeficiency virus self-testing may be used
as an alternative whilst on PrEP.
Simplifying pre-exposure prophylaxis to improve • Inconclusive HIV test results should be referred for
access and optimise use confirmatory testing.
Pre-exposure prophylaxis is safe, well tolerated and easy • Pre-exposure prophylaxis should be stopped immediately
to administer in anyone with a positive or indeterminate HIV test result.
Step 1: Check client desirability of pre-exposure prophylaxis: • Should an interruption in PrEP occur, then initiation
The aims of initiation consultations for PrEP are: testing should be performed (as above) prior to restart.
http://www.sajhivmed.org.za 68 Open Access