Page 360 - HIVMED_v21_i1.indb
P. 360
Page 3 of 5 Original Research
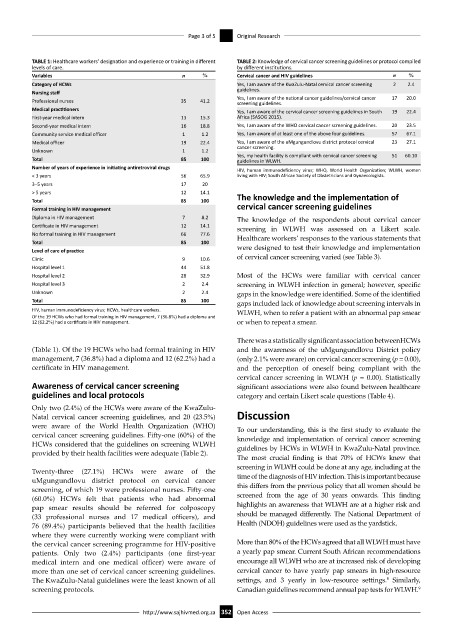
TABLE 1: Healthcare workers’ designation and experience or training in different TABLE 2: Knowledge of cervical cancer screening guidelines or protocol compiled
levels of care. by different institutions.
Variables n % Cervical cancer and HIV guidelines n %
Category of HCWs Yes, I am aware of the KwaZulu-Natal cervical cancer screening 2 2.4
Nursing staff guidelines.
Professional nurses 35 41.2 Yes, I am aware of the national cancer guidelines/cervical cancer 17 20.0
screening guidelines.
Medical practitioners Yes, I am aware of the cervical cancer screening guidelines in South 19 22.4
First-year medical intern 13 15.3 Africa (SASOG 2015).
Second-year medical intern 16 18.8 Yes, I am aware of the WHO cervical cancer screening guidelines. 20 23.5
Community service medical officer 1 1.2 Yes, I am aware of at least one of the above four guidelines. 57 67.1
Medical officer 19 22.4 Yes, I am aware of the uMgungundlovu district protocol cervical 23 27.1
Unknown 1 1.2 cancer screening.
Yes, my health facility is compliant with cervical cancer screening 51 60.10
Total 85 100 guidelines in WLWH.
Number of years of experience in initiating antiretroviral drugs HIV, human immunodeficiency virus; WHO, World Health Organization; WLWH, women
< 3 years 56 65.9 living with HIV; South African Society of Obstetricians and Gynaecologists.
3–5 years 17 20
> 5 years 12 14.1 The knowledge and the implementation of
Total 85 100
Formal training in HIV management cervical cancer screening guidelines
Diploma in HIV management 7 8.2 The knowledge of the respondents about cervical cancer
Certificate in HIV management 12 14.1 screening in WLWH was assessed on a Likert scale.
No formal training in HIV management 66 77.6 Healthcare workers’ responses to the various statements that
Total 85 100
Level of care of practice were designed to test their knowledge and implementation
Clinic 9 10.6 of cervical cancer screening varied (see Table 3).
Hospital level 1 44 51.8
Hospital level 2 28 32.9 Most of the HCWs were familiar with cervical cancer
Hospital level 3 2 2.4 screening in WLWH infection in general; however, specific
Unknown 2 2.4 gaps in the knowledge were identified. Some of the identified
Total 85 100 gaps included lack of knowledge about screening intervals in
HIV, human immunodeficiency virus; HCWs, healthcare workers. WLWH, when to refer a patient with an abnormal pap smear
Of the 19 HCWs who had formal training in HIV management, 7 (36.8%) had a diploma and
12 (62.2%) had a certificate in HIV management. or when to repeat a smear.
There was a statistically significant association betweenHCWs
(Table 1). Of the 19 HCWs who had formal training in HIV and the awareness of the uMgungundlovu District policy
management, 7 (36.8%) had a diploma and 12 (62.2%) had a (only 2.1% were aware) on cervical cancer screening (p = 0.00),
certificate in HIV management. and the perception of oneself being compliant with the
cervical cancer screening in WLWH (p = 0.00). Statistically
Awareness of cervical cancer screening significant associations were also found between healthcare
guidelines and local protocols category and certain Likert scale questions (Table 4).
Only two (2.4%) of the HCWs were aware of the KwaZulu-
Natal cervical cancer screening guidelines, and 20 (23.5%) Discussion
were aware of the World Health Organization (WHO) To our understanding, this is the first study to evaluate the
cervical cancer screening guidelines. Fifty-one (60%) of the knowledge and implementation of cervical cancer screening
HCWs considered that the guidelines on screening WLWH guidelines by HCWs in WLWH in KwaZulu-Natal province.
provided by their health facilities were adequate (Table 2).
The most crucial finding is that 70% of HCWs knew that
screening in WLWH could be done at any age, including at the
Twenty-three (27.1%) HCWs were aware of the
uMgungundlovu district protocol on cervical cancer time of the diagnosis of HIV infection. This is important because
screening, of which 19 were professional nurses. Fifty-one this differs from the previous policy that all women should be
(60.0%) HCWs felt that patients who had abnormal screened from the age of 30 years onwards. This finding
pap smear results should be referred for colposcopy highlights an awareness that WLWH are at a higher risk and
(33 professional nurses and 17 medical officers), and should be managed differently. The National Department of
76 (89.4%) participants believed that the health facilities Health (NDOH) guidelines were used as the yardstick.
where they were currently working were compliant with
the cervical cancer screening programme for HIV-positive More than 80% of the HCWs agreed that all WLWH must have
patients. Only two (2.4%) participants (one first-year a yearly pap smear. Current South African recommendations
medical intern and one medical officer) were aware of encourage all WLWH who are at increased risk of developing
more than one set of cervical cancer screening guidelines. cervical cancer to have yearly pap smears in high-resource
8
The KwaZulu-Natal guidelines were the least known of all settings, and 3 yearly in low-resource settings. Similarly,
screening protocols. Canadian guidelines recommend annual pap tests for WLWH.
9
http://www.sajhivmed.org.za 352 Open Access