Page 135 - HIVMED_v21_i1.indb
P. 135
Page 3 of 6 Original Research
All data analysis was performed using Stata version 13 Likelihood of pre-exposure prophylaxis use
(StataCorp LP, TX, USA) software package. Bivariate linear The participants’ responses when asked about the likelihood
regression was used to determine if there was a relationship of PrEP use are shown in Table 3. Regardless of a likelihood
between the RII scores of knowledge, likelihood and barriers to use PrEP, potential barriers were cited, such as stigma,
(KLBs) and exploratory factor variables that were collected costs, side-effects associated with the PrEP tablet and poor
in the study. To identify the relationship between KLB RII knowledge, as shown in Table 3.
scores, a matrix of Spearman correlation coefficients was
used.
Relative importance index
Ethical consideration On a scale of RII, the median score for PrEP knowledge
was ‘0’, indicating that participants had limited knowledge
Prior to conducting the survey, the study protocol including about PrEP. Participants perceived the use of PrEP as an
the data collecting tool was reviewed and approved by important component in the ideal HIV prevention strategy
the Joint Research Ethics Committee of the University of once educated about it. In relation to the likelihood of
Zimbabwe and the Parirenyatwa Group of Hospitals PrEP use, the median score for the likelihood of PrEP use
(JREC/328/16). All participants provided written informed was 0.89 ranging from 0.48 to 1. Therefore, the likelihood
consent before participating in the study. of PrEP use amongst the participants was high. The
RII median score for barriers associated with PrEP use
Results was 0.29 (IQR: 0–0.63). This indicated that the barriers
associated with PrEP uptake were less likely than
A total of 131 presumed HIV-negative, adult FSWs were
recruited to participate in this study, and their demographic knowledge to affect participants’ use of PrEP. Results that
characteristics are shown in Table 1. All study participants were statistically significant in the bivariate analysis are
were self-identified as residents of the Harare province. shown in Table 4.
Participant’s characteristics – Sexual risk factors An increase in the number of dependents was associated
and human immunodeficiency virus testing with a reduced knowledge about PrEP, as shown in Table 4.
There was a statistically significant association between age
The median number of sexual encounters by the participants and likelihood of PrEP use. As participants became older,
was five [interquartile range (IQR): 3–6] partners per there was an increase in the likelihood of PrEP use. This
day. Half of the participants (50%) did not know increased amongst participants who had unprotected sex in
their partner’s HIV serostatus and only 42% of the FSWs the last 3 months.
would talk about HIV with their clients or partners. All
participants perceived the use of condoms as a necessary There was, however, no statistically significant association
tool when engaging in sexual activity with their partners between knowledge RII with age, marital status, education,
or clients, 86% used condoms with the last three partners change in place of residence, income and years of practice as
they encountered and 44% reported having ever had a a sex worker (p > 0.05).
condom burst at least once during sexual intercourse.
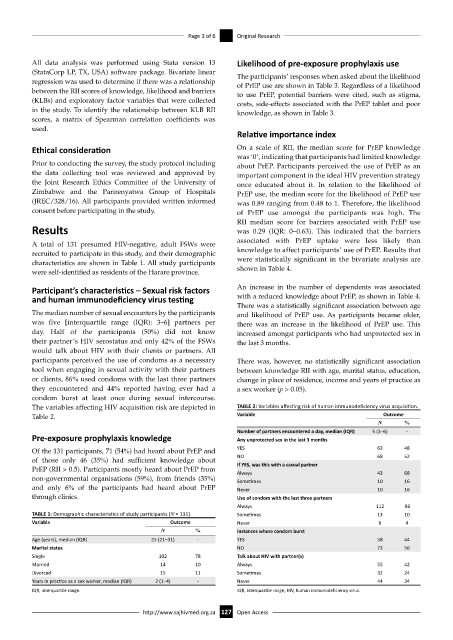
The variables affecting HIV acquisition risk are depicted in TABLE 2: Variables affecting risk of human immunodeficiency virus acquisition.
Table 2. Variable Outcome
N %
Number of partners encountered a day, median (IQR) 5 (3–6) -
Pre-exposure prophylaxis knowledge Any unprotected sex in the last 3 months
Of the 131 participants, 71 (54%) had heard about PrEP and YES 63 48
of those only 46 (35%) had sufficient knowledge about NO 68 52
If YES, was this with a casual partner
PrEP (RII > 0.5). Participants mostly heard about PrEP from Always 43 68
non-governmental organisations (59%), from friends (35%) Sometimes 10 16
and only 6% of the participants had heard about PrEP Never 10 16
through clinics. Use of condom with the last three partners
Always 112 86
TABLE 1: Demographic characteristics of study participants (N = 131). Sometimes 13 10
Variable Outcome Never 6 4
N % Instances where condom burst
Age (years), median (IQR) 25 (21–31) - YES 58 44
Marital status NO 73 56
Single 102 78 Talk about HIV with partner(s)
Married 14 10 Always 55 42
Divorced 15 11 Sometimes 32 24
Years in practice as a sex worker, median (IQR) 2 (1–4) - Never 44 34
IQR, interquartile range. IQR, interquartile range; HIV, human immunodeficiency virus.
http://www.sajhivmed.org.za 127 Open Access