Page 70 - HIVMED_v21_i1.indb
P. 70
Page 5 of 8 Guideline
defined, but commencing therapy 2–3 days prior to to > 150 000 copies/µL, and none of the recipients to date
transplantation should provide adequate time for the have developed virological failure from a transmitted strain
drugs to achieve steady state at the time of transplantation of HIV. 39,42 For donors with an unsuppressed VL, we
(i.e. approximately 4 half-lives of the drug). recommend that the recipient should be placed on an ART
• We currently suggest continuing ART indefinitely. Any regimen that would be expected to treat both their own and
decision to stop ART at a later stage should only be made the donor’s HIV strains. Consultation with an infectious
if, despite intensive testing (including with highly diseases specialist experienced in managing transplant
sensitive assays), there is still no clear evidence that HIV patients is mandatory.
transmission took place, and this should only be
undertaken after informed consent and with the approval Care of the human
of the HREC overseeing the case. immunodeficiency virus-positive
recipient after transplantation
Donor eligibility
For the most part, we recommend routine HIV care post-
Living human immunodeficiency virus-positive donor transplantation, with minor alterations where indicated:
• Standard living donor work-up • In view of the potential for unanticipated treatment
• Duration of ART ≥ 3 months interruptions and drug–drug interactions, we recommend
+
• CD4 count ≥ 200 cells/µL (cluster of differentiation performing an HIV VL measurement within 2–3 months
4 T-cell percentage [CD4 %] ≥ 15% for patients aged after transplantation. A VL > 50 copies/µL should prompt
+
< 5 years) urgent intervention as per the latest Southern African
• Plasma VL < 50 copies/µL HIV Clinicians Society Guidelines.
• The recipient must be able to receive a safe and effective • Key drug–drug interactions are outlined in Table 1.
ART regimen, considering the donor’s anticipated HIV Physicians should be aware of these and consider
viral resistance strains. changing therapy accordingly if required. In general,
InSTI-based ART offers the fewest drug–drug interactions
Rationale: The prospective donor must have demonstrated with commonly used immunosuppressant drugs, as
durable and stable control of their HIV, to minimise the risk well as a high barrier to resistance.
of unmasking IRIS reactions occurring subsequent to organ • HIV-positive transplant recipients should receive the
donation, which could jeopardise the health of the donor. same vaccines as HIV-negative transplant recipients.
A CD4 threshold ≥ 200 cells/µL is also recommended to • HIV-positive transplant recipients should receive the
+
minimise the likelihood of occult opportunistic infections same post-transplantation prophylaxis for opportunistic
either manifesting after organ recovery or being transmitted infections as HIV-negative transplant recipients.
to the donor during transplantation. We do not consider
a pre-transplantation biopsy of the donor organ to be a Ethical consideration
routine requirement merely because of HIV infection.
In all cases, the decision to receive an organ from an HIV-
positive donor should be made freely and without
Deceased human immunodeficiency virus-positive donor coercion. In addition, potential organ recipients should be
made aware of the possibility of receiving an organ from an
• Standard criteria, as for HIV-negative deceased donors. HIV-negative donor. In the case of children who received
• For deceased donors with a history of HIV resistance or HIV-positive donor organs and have not reached the age of
virological failure, the recipient must be able to receive a consent, every effort must be made to ensure the protection
safe, tolerable and effective ART regimen considering the of their best interests.
donor’s known or inferred patterns of viral resistance.
Adult recipients of organs from HIV-positive donors and
Rationale: Although the risk of transmission of the donor caregivers of child recipients must be made aware of the
virus to the recipient is likely to be higher if the donor has importance of adherence to antiretroviral medication, and
an unsuppressed VL, limiting the deceased donor pool only the complexities inherent in this type of transplant. To this
to virally suppressed individuals would significantly end, a social worker should be an integral part of the
restrict the number of organs available. Deceased donors transplant team involved in donor and recipient assessment,
in South Africa had VLs that ranged from undetectable and this person should be in a position to empower potential
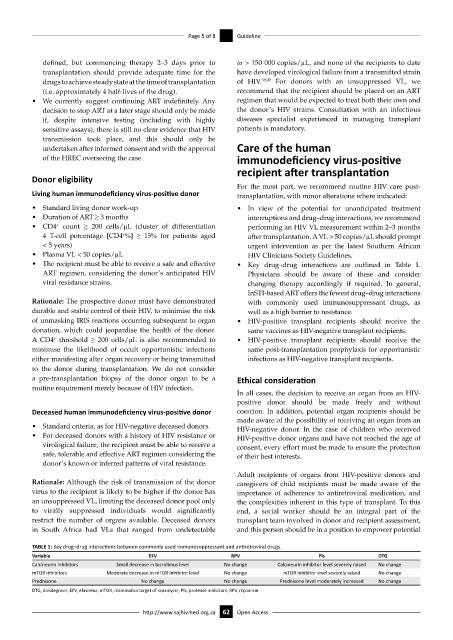
TABLE 1: Key drug–drug interactions between commonly used immunosuppressant and antiretroviral drugs.
Variable EFV RPV PIs DTG
Calcineurin inhibitors Small decrease in tacrolimus level No change Calcineurin inhibitor level severely raised No change
mTOR inhibitors Moderate decrease in mTOR inhibitor level No change mTOR inhibitor level severely raised No change
Prednisone No change No change Prednisone level moderately increased No change
DTG, dolutegravir; EFV, efavirenz; mTOR, mammalian target of rapamycin; PIs, protease inhibitors; RPV, rilpivirine.
http://www.sajhivmed.org.za 62 Open Access